Table of Contents
- Introduction: A Pragmatic Guide to AI in Clinical Practice
- The Current Clinical Landscape and Pressing Challenges
- Core AI Methods Explained for Clinicians
- Practical Clinical Applications of Artificial Intelligence in Healthcare
- Integrating AI into Clinical Workflows: A Stepwise Roadmap for 2025 and Beyond
- Data Governance, Privacy, and Ethical Safeguards
- Validation, Safety, and Performance Monitoring
- Measuring Clinical Outcomes and Value
- Operational Barriers and Change Management
- Concise Case Studies with Measurable Outcomes
- Future Trends and Readiness Checklist
- Resources and References
Introduction: A Pragmatic Guide to AI in Clinical Practice
The conversation around Artificial Intelligence in Healthcare is often dominated by futuristic hype, obscuring the practical realities of implementation. This whitepaper moves beyond speculation to provide a pragmatic guide for clinicians, health system leaders, and technology strategists. Our focus is not on technology for its own sake, but on its potential to address real-world clinical challenges when thoughtfully integrated into existing workflows. We will explore how to harness AI to improve patient outcomes, enhance operational efficiency, and support clinical decision-making, all while navigating the critical ethical and governance guardrails.
Purpose and Scope of this Whitepaper
The purpose of this document is to demystify AI for a clinical audience. We will break down core concepts, showcase tangible applications, and provide a clear roadmap for adoption. The scope is centered on the operational and clinical aspects of implementation, including workflow integration, validation, change management, and measuring true value. We will prioritize evidence over excitement, offering a balanced view of the opportunities and challenges that define the current state of Artificial Intelligence in Healthcare.
The Current Clinical Landscape and Pressing Challenges
Healthcare systems today face a confluence of pressures. Rising operational costs, an aging population with complex comorbidities, and an unprecedented level of clinician burnout demand innovative solutions. The integration of Artificial Intelligence in Healthcare is not a luxury but an emerging necessity to address these systemic issues.
Navigating Clinician Burnout and Data Overload
Clinicians are inundated with data from electronic health records (EHRs), imaging studies, lab results, and patient-generated health data. This data deluge contributes significantly to cognitive burden and administrative tasks, pulling focus away from direct patient care. AI offers a pathway to automate routine tasks, synthesize complex data into actionable insights, and reduce the documentation burden that is a primary driver of burnout.
The Imperative for Value-Based Care
The paradigm shift from fee-for-service to value-based care models requires a proactive, predictive, and personalized approach to medicine. Success in this new landscape depends on the ability to identify at-risk patients, optimize treatment pathways, and prevent adverse events before they occur. AI-powered analytics are uniquely suited to meet these demands by enabling more accurate risk stratification and resource allocation.
Core AI Methods Explained for Clinicians
Understanding the foundational methods of AI is crucial for evaluating and implementing these technologies responsibly. For clinicians, it is less important to know the complex mathematics and more important to understand what each method does and where it can be applied.
Machine Learning (ML)
Machine Learning is a subset of AI where algorithms are trained on large datasets to recognize patterns and make predictions without being explicitly programmed for that specific task. In a clinical context, an ML model could be trained on thousands of patient records to predict the likelihood of sepsis based on a combination of vital signs and lab results.
- Supervised Learning: The algorithm learns from labeled data (e.g., chest X-rays labeled as “pneumonia” or “no pneumonia”) to make predictions on new, unlabeled data.
- Unsupervised Learning: The algorithm identifies hidden patterns in unlabeled data, which can be used to discover novel patient subgroups or phenotypes.
Deep Learning (DL)
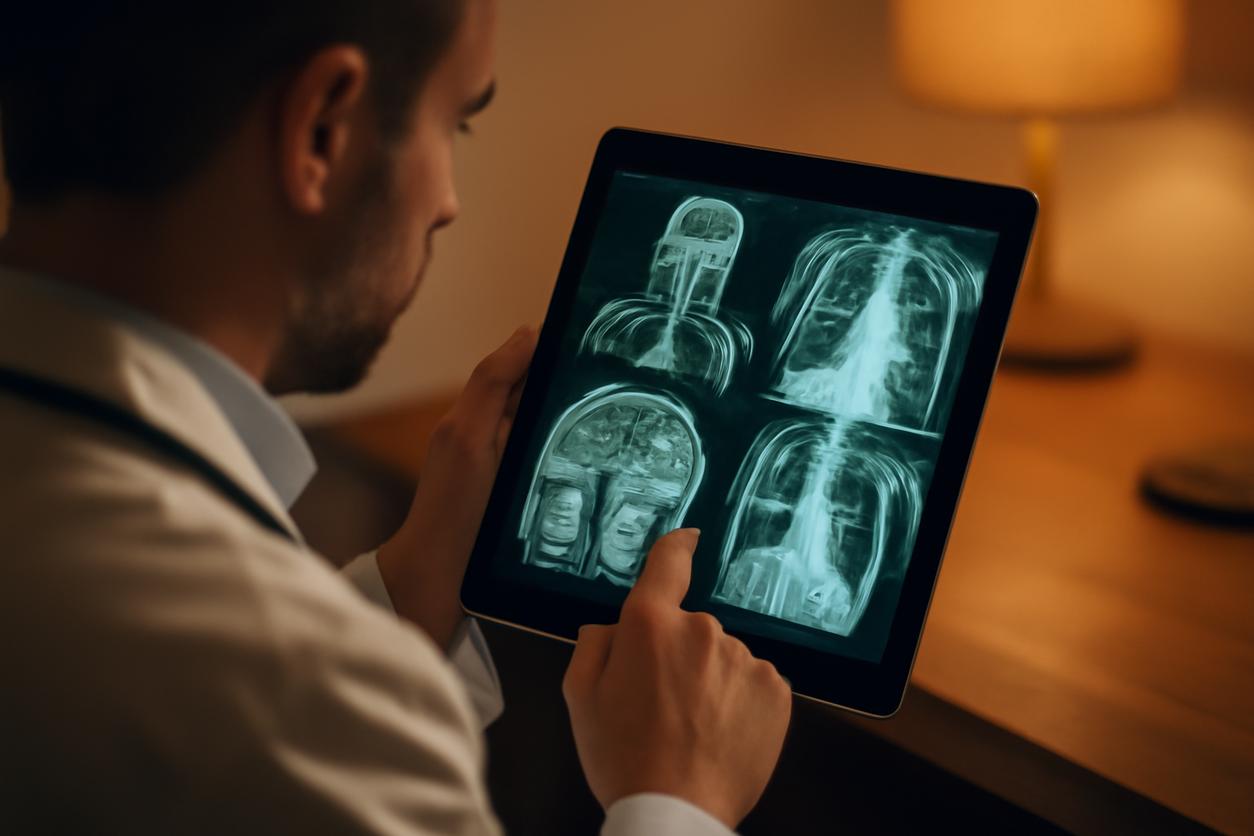
Deep Learning is an advanced form of machine learning that uses multi-layered neural networks, inspired by the human brain. It excels at recognizing intricate patterns in large, unstructured datasets like medical images or genomic sequences. A key application is in radiology, where deep learning models can detect subtle abnormalities in CT scans or mammograms that may be missed by the human eye.
Natural Language Processing (NLP)
Natural Language Processing gives computers the ability to understand, interpret, and generate human language. In healthcare, NLP is critical for unlocking the vast amount of unstructured data trapped in clinical notes, pathology reports, and scientific literature. It can be used to extract specific clinical concepts from physician notes, summarize patient histories, or power voice-activated clinical assistants.
Practical Clinical Applications of Artificial Intelligence in Healthcare
The true measure of Artificial Intelligence in Healthcare is its ability to deliver tangible benefits within clinical practice. The following are established and emerging applications that are already making an impact.
Enhancing Diagnostic Accuracy
AI algorithms, particularly deep learning models, are increasingly used as a second reader or a decision support tool in diagnostic specialties. Key examples include:
- Radiology: Detecting early-stage cancers in mammograms, identifying strokes on brain CT scans, and quantifying lung disease from chest X-rays.
- Pathology: Assisting pathologists in grading tumors and identifying cancerous cells on digital slides, improving consistency and efficiency.
- Cardiology: Analyzing ECGs to detect arrhythmias or predicting the risk of future cardiovascular events from echocardiograms.
Personalizing Treatment Planning
AI can synthesize diverse patient data—including genomics, proteomics, clinical history, and lifestyle factors—to help clinicians tailor treatment plans for individual patients. In oncology, for example, AI platforms can analyze a tumor’s molecular profile to recommend the most effective targeted therapies or clinical trials, moving medicine closer to a truly personalized approach.
Revolutionizing Remote Patient Monitoring
With the rise of wearable sensors and at-home medical devices, AI is becoming essential for managing the continuous stream of data from patients with chronic conditions like diabetes, hypertension, or heart failure. AI algorithms can detect subtle deteriorations in a patient’s condition, alert care teams to potential issues, and predict exacerbations, enabling timely interventions that can prevent hospitalizations.
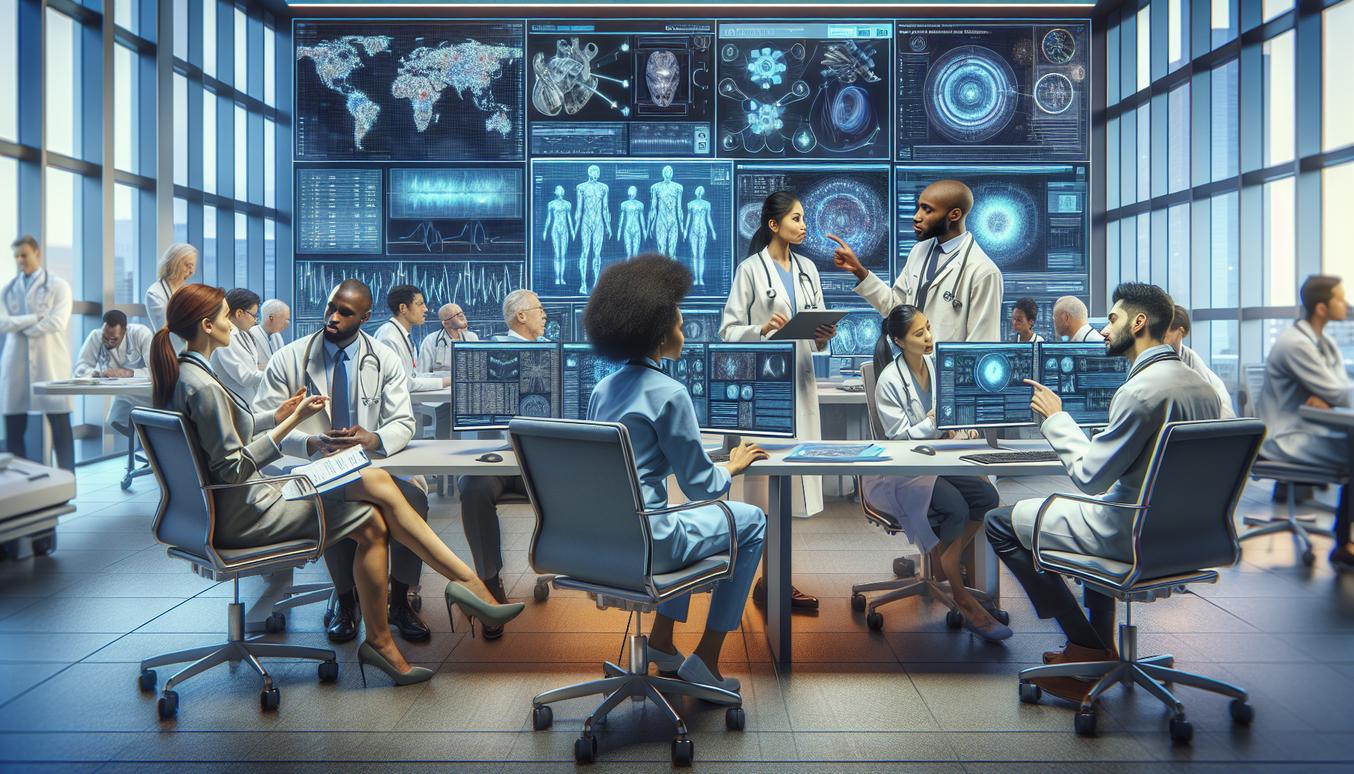
Integrating AI into Clinical Workflows: A Stepwise Roadmap for 2025 and Beyond
Successful AI adoption is not a technology project; it is a clinical transformation initiative. A phased, clinician-centric approach is essential. The following strategies for 2025 and onward prioritize safety, efficacy, and seamless integration.
Phase 1: Problem Identification and Use Case Selection
Begin by identifying a high-impact clinical problem that is well-suited for an AI solution. Engage frontline clinicians to pinpoint workflow bottlenecks or areas of diagnostic uncertainty. Prioritize use cases with clear success metrics and a strong potential for improving patient outcomes or operational efficiency.
Phase 2: Pilot Implementation and Workflow Analysis
Deploy the AI tool in a limited, controlled pilot environment. The primary goal is to study its impact on the clinical workflow integration. Observe how clinicians interact with the tool. Does it add steps? Does it provide information at the right time and in the right format? Gather feedback and iterate before considering a broader rollout.
Phase 3: Scaled Deployment and Continuous Optimization
Once the AI tool is validated and refined, plan for a scaled deployment. This requires comprehensive training, clear communication about the tool’s capabilities and limitations, and a robust technical support structure. Implementation is not the end goal; it is the beginning of a continuous cycle of monitoring, evaluation, and optimization.
Data Governance, Privacy, and Ethical Safeguards
Trust is the cornerstone of healthcare. The use of Artificial Intelligence in Healthcare must be underpinned by a rigorous commitment to data governance, patient privacy, and ethical principles.
Building a Robust Data Governance Framework
A formal governance structure is non-negotiable. This includes establishing clear policies for data quality, security, and lifecycle management. It is essential to ensure that the data used to train and validate AI models is accurate, complete, and representative of the patient population it will serve.
Upholding Patient Privacy and Consent
All AI initiatives must comply with data privacy regulations like HIPAA. This involves using de-identified or anonymized data wherever possible and implementing strong access controls. Furthermore, healthcare organizations should be transparent with patients about how their data is being used and establish clear consent processes.
Addressing Algorithmic Bias and Fairness
AI models are susceptible to learning and amplifying biases present in historical data. If a training dataset underrepresents certain demographic groups, the resulting algorithm may perform poorly for those populations. It is a clinical and ethical imperative to proactively audit models for algorithmic bias and ensure they produce equitable outcomes across all patient groups.
Validation, Safety, and Performance Monitoring
An AI algorithm intended for clinical use is a medical tool and must be subjected to the same level of scrutiny as any other medical device or intervention.
The Necessity of Clinical Validation
Before deployment, an AI model must be rigorously validated on a local, independent dataset that reflects the organization’s specific patient population and clinical environment. Retrospective validation is a start, but prospective clinical studies, as documented in sources like PubMed, provide the highest level of evidence for safety and efficacy.
Continuous Performance Monitoring Post-Deployment
An AI model’s performance can degrade over time due to shifts in patient populations, clinical practices, or data acquisition methods. This phenomenon, known as “model drift,” necessitates a program for continuous performance monitoring. Organizations must track key metrics and have a plan to retrain or recalibrate models as needed to ensure ongoing safety and accuracy.
Measuring Clinical Outcomes and Value
The ultimate success of any AI initiative is measured not by its technical sophistication but by its impact on clinical care and operational efficiency. Organizations must define and track key performance indicators (KPIs) to demonstrate value.
Key Performance Indicators (KPIs) for AI in Healthcare
- Clinical Outcomes: Reductions in mortality rates, complication rates, length of stay, or hospital readmissions. Improvements in diagnostic accuracy or time to diagnosis.
- Operational Efficiency: Reductions in clinician administrative time, improvements in patient throughput, or optimization of resource utilization (e.g., operating room scheduling).
- Financial Impact: Reductions in the total cost of care, improved performance in value-based care contracts, or reduced claim denials.
Operational Barriers and Change Management
Implementing Artificial Intelligence in Healthcare is a complex endeavor with significant operational hurdles.
Overcoming Technical and Data-Related Hurdles
Common challenges include poor data quality, lack of interoperability between systems, and the high cost of data infrastructure. A successful strategy requires a long-term investment in creating a clean, standardized, and accessible data ecosystem.
Fostering Clinical Adoption and Trust
The most significant barrier is often cultural, not technical. Clinicians may be skeptical of “black box” algorithms or fear being replaced. Effective change management is critical. This includes:
- Engaging Clinicians Early and Often: Involve clinicians in the selection, validation, and workflow design process.
- Providing Comprehensive Education: Train users not just on how to use the tool, but on its underlying principles, strengths, and limitations.
- Promoting a Culture of Augmentation: Frame AI as a tool that augments and supports clinical expertise, rather than replacing it.
Concise Case Studies with Measurable Outcomes
The following table illustrates the practical impact of well-integrated AI solutions.
| Clinical Problem | AI Intervention | Measurable Outcomes |
|---|---|---|
| Delayed Sepsis Detection | An EHR-integrated machine learning algorithm that continuously monitors patient data for early signs of sepsis and alerts the rapid response team. |
|
| High Hospital Readmission Rates for Heart Failure | An NLP tool that analyzes discharge summaries to identify patients at high risk for readmission, combined with an RPM platform to monitor them post-discharge. |
|
| Radiologist Burnout and Backlog | A deep learning-based triage tool that analyzes chest X-rays upon acquisition and prioritizes studies with critical findings for immediate review. |
|
Future Trends and Readiness Checklist
The field of Artificial Intelligence in Healthcare is evolving rapidly. Staying prepared requires an understanding of emerging trends and an honest assessment of organizational readiness.
Emerging Trends in Healthcare AI
- Generative AI: Large language models (LLMs) are being explored to automate clinical documentation, summarize patient encounters, and even draft patient communications.
- Federated Learning: A technique that allows AI models to be trained across multiple institutions without centralizing sensitive patient data, addressing privacy and data-sharing challenges.
- Digital Twins: The creation of virtual, dynamic models of patients or physiological systems, which can be used to simulate disease progression and test therapeutic interventions before applying them in the real world.
Organizational Readiness Checklist
Before embarking on a major AI initiative, leaders should assess their organization’s readiness:
- Leadership and Vision: Is there executive sponsorship and a clear strategic vision for how AI will support clinical and business goals?
- Data Infrastructure: Do you have access to high-quality, integrated data and the technical infrastructure to support AI models?
- Clinical Engagement: Are clinicians actively involved and supportive of adopting new technologies?
- Governance and Ethics: Is there a formal committee or framework in place to oversee the ethical and responsible implementation of AI?
- Talent and Expertise: Do you have in-house or partner expertise in data science, clinical informatics, and change management?
Resources and References
For health system leaders and clinicians seeking to deepen their understanding of Artificial Intelligence in Healthcare, the following resources provide authoritative information, research, and global health perspectives.
- World Health Organization (WHO): Offers guidance on the ethics and governance of artificial intelligence for health.
- National Institutes of Health (NIH): Funds and conducts extensive research on the application of AI in biomedical science and clinical care.
- PubMed: A comprehensive database of biomedical literature for finding peer-reviewed studies on the clinical validation of AI tools.
- Nature Medicine: A leading journal that frequently publishes cutting-edge research on the intersection of technology and clinical medicine.