A Pragmatic Guide to Artificial Intelligence in Healthcare: From Pilots to Clinical Practice
Table of Contents
- Introduction: Why AI Matters in Modern Clinical Practice
- Overview of Core AI Techniques Used in Healthcare
- Neural Networks and Medical Imaging
- Predictive Modeling for Patient Risk and Outcomes
- Natural Language Processing in Clinical Notes
- Integrating AI into Clinical Workflows
- Assessment: Validation, Metrics and Clinical Impact
- Governance, Ethics and Bias Mitigation
- Designing Effective Pilots and Scaling Safely
- Common Implementation Pitfalls and How to Avoid Them
- Emerging Research Directions and Opportunities
- Glossary of Key Terms and Further Reading
Introduction: Why AI Matters in Modern Clinical Practice
The integration of Artificial Intelligence in Healthcare has moved from theoretical discussions to tangible applications that are reshaping clinical practice. For clinicians, hospital administrators, and data scientists, AI is no longer a distant concept but a powerful tool to enhance diagnostic accuracy, personalize patient treatment, and streamline operational efficiency. The core promise of AI in this sector is not to replace the expertise of healthcare professionals but to augment their capabilities, allowing them to manage overwhelming data volumes and derive insights that were previously inaccessible. By automating routine tasks and identifying subtle patterns in complex datasets, Artificial Intelligence in Healthcare helps providers focus on what matters most: direct patient care and complex decision-making.
This comprehensive guide provides a pragmatic roadmap for understanding and implementing AI solutions. We will move beyond the hype to focus on practical steps, from data preparation and pilot design to ethical governance and measuring real-world impact. The goal is to equip healthcare leaders with the knowledge to navigate the complexities of AI adoption, ensuring that technology serves clinical excellence and improves patient outcomes.
Overview of Core AI Techniques Used in Healthcare
Understanding the fundamental technologies driving Artificial Intelligence in Healthcare is the first step toward effective implementation. While the field is vast, a few core techniques form the backbone of most current medical AI applications. These methods are designed to process different types of health data, from images to text to structured electronic health records, each offering unique capabilities to solve clinical challenges.
Neural Networks and Medical Imaging
At the forefront of medical image analysis are Artificial Neural Networks, particularly a subset known as deep learning. These algorithms are exceptionally skilled at recognizing intricate patterns, making them ideal for radiology, pathology, and ophthalmology. By training on thousands of labeled images, these models learn to identify anomalies with a high degree of accuracy.
- Radiology: AI algorithms can screen mammograms for signs of breast cancer or analyze CT scans to detect lung nodules, often highlighting areas of concern for a radiologist to review. This serves as a powerful second reader, reducing the risk of missed diagnoses and speeding up interpretation times.
- Pathology: In digital pathology, AI can analyze tissue slide images to identify and count cancerous cells, grade tumors, and predict molecular markers, tasks that are time-consuming and subject to inter-observer variability when done manually.
- Ophthalmology: Models can diagnose conditions like diabetic retinopathy or age-related macular degeneration from retinal fundus images, enabling early detection and intervention, especially in underserved areas.
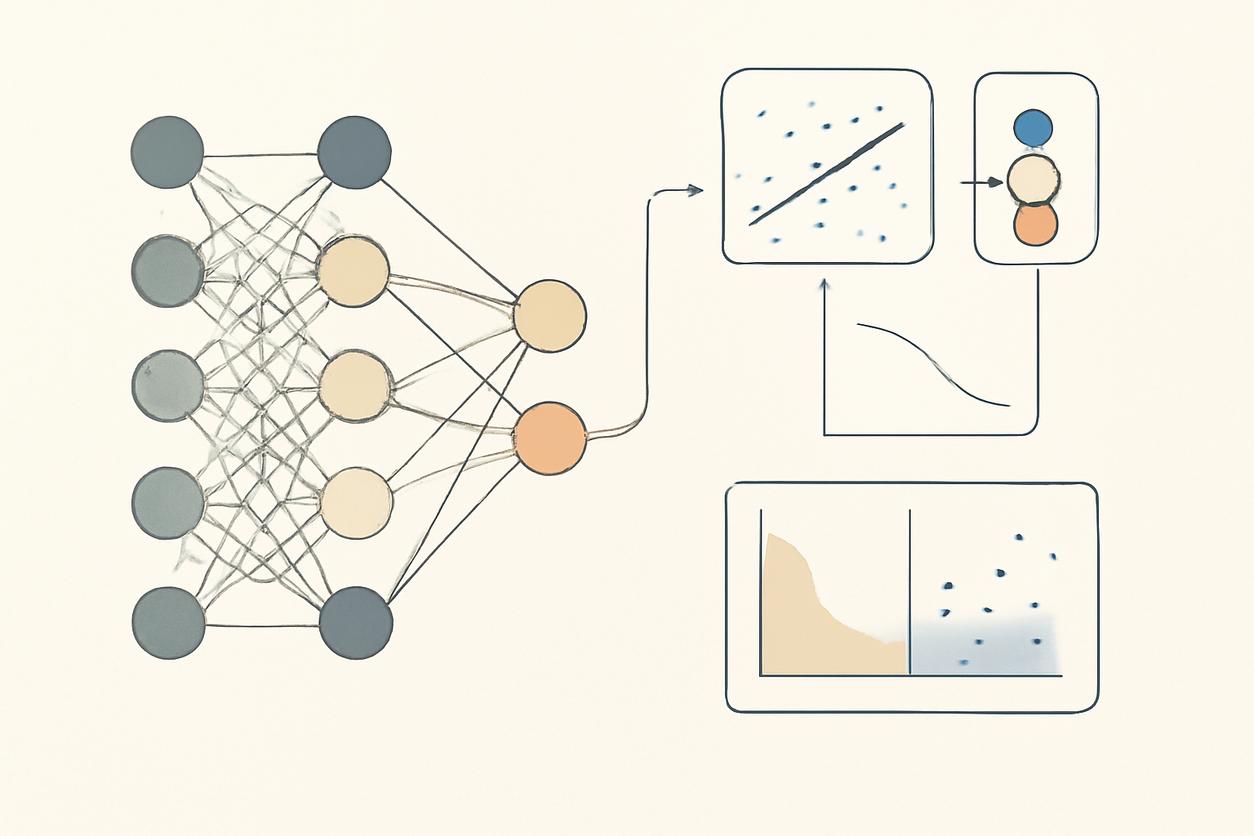
Predictive Modeling for Patient Risk and Outcomes
Predictive modeling uses machine learning algorithms to analyze historical patient data and forecast future events. These models leverage vast datasets from Electronic Health Records (EHRs), genomic data, and wearable device streams to identify patients at high risk for specific conditions, allowing for proactive intervention.
Key applications include:
- Sepsis Prediction: AI systems can monitor patient vitals and lab results in real-time to predict the onset of sepsis hours before it becomes clinically apparent, enabling earlier treatment.
- Readmission Risk: Hospitals use predictive models to identify patients with a high probability of being readmitted within 30 days of discharge, allowing care teams to allocate additional resources and follow-up care.
- Treatment Response: By analyzing a patient’s clinical and genetic profile, AI can help predict their likely response to a particular drug or therapy, paving the way for personalized medicine.
Natural Language Processing in Clinical Notes
A significant portion of critical patient information is locked away in unstructured text, such as clinician notes, discharge summaries, and pathology reports. Natural Language Processing (NLP) is the branch of AI that enables computers to understand and extract meaningful information from human language.
Practical uses in a clinical context involve:
- Data Extraction: NLP can scan through thousands of clinical notes to identify patient cohorts with specific symptoms, diagnoses, or outcomes for clinical research.
- Clinical Documentation Improvement (CDI): AI tools can analyze notes to suggest more specific medical codes, ensuring accurate billing and quality reporting.
- Pharmacovigilance: Health systems can use NLP to monitor EHRs for mentions of adverse drug reactions, helping to identify safety signals much faster than traditional reporting methods.
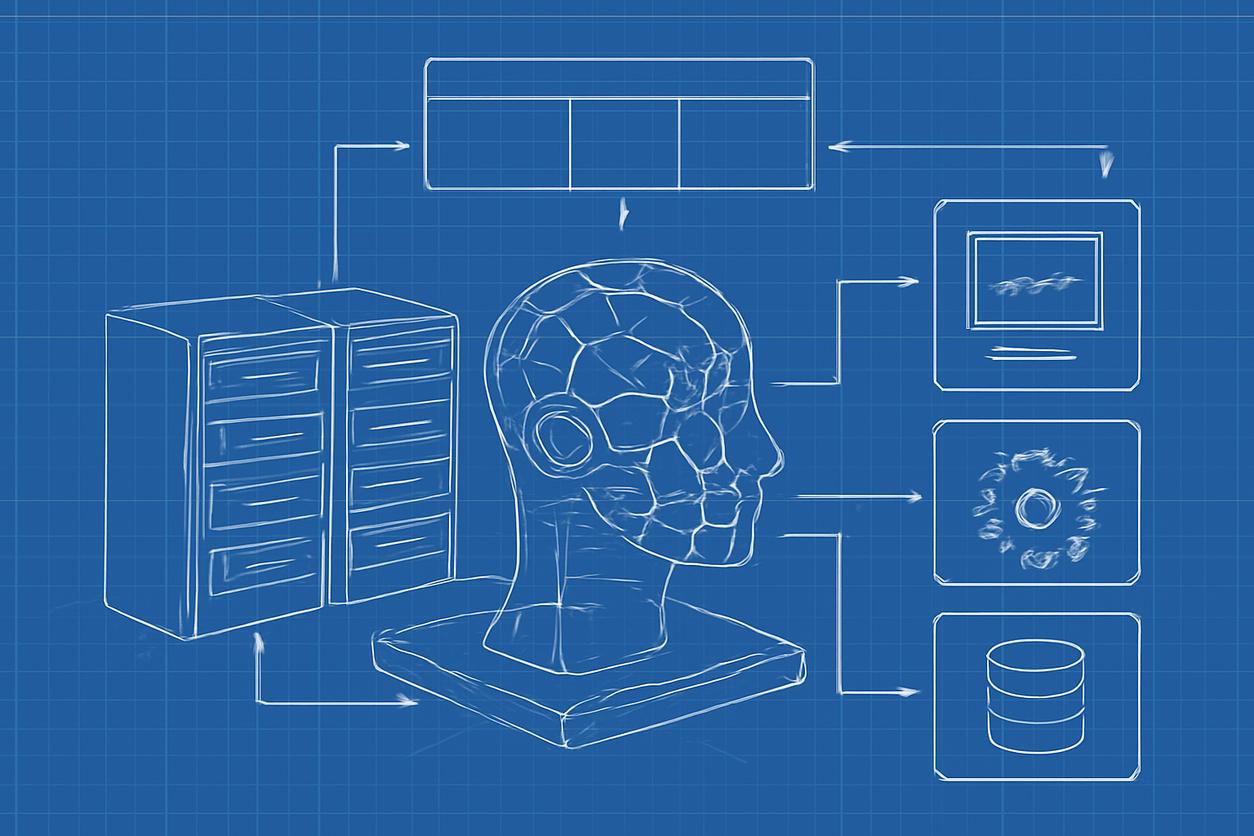
Integrating AI into Clinical Workflows
A brilliant algorithm is clinically useless if it cannot be seamlessly integrated into the daily workflows of healthcare professionals. Successful implementation of Artificial Intelligence in Healthcare depends as much on thoughtful integration and human-centric design as it does on the underlying technology itself.
Data Readiness, Interoperability and Pipelines
The performance of any AI model is fundamentally limited by the quality and accessibility of the data it is trained on. Before an algorithm can be deployed, healthcare organizations must address several data-related prerequisites.
- Data Quality: Data must be accurate, complete, and consistent. This often requires significant effort in data cleaning and preprocessing.
- Interoperability: Data often resides in siloed systems (EHRs, PACS, lab systems). Adopting standards like FHIR (Fast Healthcare Interoperability Resources) is crucial for creating a unified data pipeline that AI models can access.
- Robust Pipelines: An automated, reliable data pipeline is necessary to feed real-time data to AI models and deliver their outputs back to the clinical workflow in a timely manner.
Human in the Loop: Roles and Responsibilities
Effective AI systems in healthcare are not autonomous decision-makers; they are assistive tools. The “human-in-the-loop” model ensures that a qualified clinical professional is always involved in validating, interpreting, and acting upon AI-generated insights. This approach builds trust, maintains clinical accountability, and provides a crucial safety net.
This model establishes clear roles:
- The AI model provides a prediction, classification, or recommendation.
- The clinician reviews the AI’s output in the context of the full clinical picture, using their judgment and expertise to make the final decision.
- This interaction also generates valuable feedback that can be used to monitor and retrain the model over time, improving its performance.
Assessment: Validation, Metrics and Clinical Impact
Deploying an AI model is not the end of the journey. Rigorous and continuous assessment is essential to ensure it is safe, effective, and delivering real value. Evaluation must go beyond standard technical metrics like accuracy or precision. While these are important for initial validation, the true test of an AI tool is its impact in a live clinical setting. Organizations must ask: Does the tool improve diagnostic accuracy? Does it lead to better patient outcomes? Does it reduce clinician burnout by saving time? Measuring these clinical and operational impacts requires well-designed prospective studies and a clear definition of success metrics before deployment.
Governance, Ethics and Bias Mitigation
The power of Artificial Intelligence in Healthcare comes with significant responsibilities. A robust governance framework is non-negotiable for ensuring that AI tools are used ethically, equitably, and safely. This involves establishing clear policies for data handling, model validation, and ongoing monitoring.
A primary ethical concern is algorithmic bias. If a model is trained on data from a specific demographic, it may perform poorly and unfairly for underrepresented populations. Mitigation strategies include auditing training datasets for representativeness, testing model performance across different demographic subgroups, and incorporating fairness metrics into the evaluation process. Transparency and explainability (XAI) are also key, as clinicians need to understand, at least to some degree, why a model reached a particular conclusion to trust its output.
Privacy and Security Best Practices
AI systems process immense amounts of Protected Health Information (PHI), making security and privacy paramount. All AI applications must be designed for compliance with regulations like HIPAA in the United States or GDPR in Europe.
- Data Minimization: Use only the minimum amount of data necessary to train and run the model.
- Anonymization and De-identification: Remove direct patient identifiers from data wherever possible.
- Secure Infrastructure: Deploy AI systems on secure, access-controlled platforms, whether on-premise or in the cloud.
- Federated Learning: An emerging technique where the AI model is sent to the data’s location (e.g., a hospital) to train locally. This allows multiple institutions to collaborate on building a robust model without sharing sensitive patient data.
Regulatory Considerations and Compliance
Many AI tools used for diagnosis or treatment recommendations are classified as Software as a Medical Device (SaMD) and are subject to oversight by regulatory bodies like the U.S. Food and Drug Administration (FDA). Gaining regulatory clearance requires comprehensive documentation of the model’s design, validation data, and performance. Organizations must also have a plan for post-market surveillance to monitor the model’s performance in the real world and manage any updates or changes, a concept known as “Good Machine Learning Practice” (GMLP).
Designing Effective Pilots and Scaling Safely
Successful enterprise-wide adoption of AI begins with a well-designed pilot project. The key is to start with a narrow, clearly defined clinical problem where AI can offer a tangible benefit. Involving end-users—physicians, nurses, and technicians—from the very beginning is critical for ensuring the solution is practical and integrates smoothly into their existing workflows. The pilot phase should be treated as a learning experience, with a focus on gathering feedback, iterating on the design, and rigorously measuring outcomes before considering a broader rollout.
Measuring ROI and Patient Centric Outcomes
The Return on Investment (ROI) for Artificial Intelligence in Healthcare extends far beyond direct financial gains. While cost savings from improved efficiency are important, the primary focus should be on clinical and patient-centric outcomes.
Key metrics should include:
- Clinical Outcomes: Reduced mortality rates, lower complication rates, improved diagnostic accuracy.
- Operational Efficiency: Decreased patient length of stay, reduced clinician documentation time, optimized operating room scheduling.
- Patient Experience: Improved patient satisfaction scores, better access to care.
Looking ahead, a key strategy for 2025 and beyond will be to directly link AI initiatives to value-based care models. This involves demonstrating how an AI tool contributes to achieving better patient outcomes at a lower overall cost. Another forward-looking strategy, expected to mature by 2026, involves establishing federated validation networks, where new AI models can be tested across multiple health systems on diverse patient populations before deployment, ensuring they are robust, equitable, and generalizable.
Common Implementation Pitfalls and How to Avoid Them
Many AI projects in healthcare fail not because of flawed technology, but due to strategic and operational missteps. Awareness of these common pitfalls can significantly increase the chances of success.
- Vague Problem Definition: Avoid a “technology-first” approach. Instead of saying “we need an AI strategy,” start with a specific clinical problem, such as “how can we reduce the time to diagnosis for stroke patients in the ER?”
- Ignoring Workflow Integration: The most accurate model will be abandoned if it is cumbersome to use. Involve clinical end-users throughout the design process to ensure the tool fits their needs.
- Underestimating Data Work: It is often said that 80% of an AI project is data preparation. Allocate sufficient time and resources for data cleaning, normalization, and pipeline construction.
- Lack of Clinical Buy-In: Engage clinical champions early and often. Their involvement is crucial for validating the tool, building trust among peers, and driving adoption.
- Forgetting Model Maintenance: AI models can degrade over time as clinical practices or patient populations change, a phenomenon known as “model drift.” Implement a system for continuous monitoring and periodic retraining.
Emerging Research Directions and Opportunities
The field of Artificial Intelligence in Healthcare is evolving rapidly. Several emerging areas hold immense promise for the future. Generative AI is being explored for creating synthetic health data, which can be used to train robust models without compromising patient privacy. Another major frontier is multimodal AI, which integrates diverse data types—such as medical images, genomic sequences, pathology reports, and clinical notes—to create a holistic, 360-degree view of the patient. This approach promises to unlock deeper insights and enable more precise and personalized medicine. For those interested in the cutting edge of research, resources from organizations like the Nature AI Topic page and the NIH offer a window into the latest breakthroughs.
Glossary of Key Terms and Further Reading
- Algorithm: A set of rules or instructions given to a computer to solve a problem or perform a task.
- Bias: A systematic error in an AI model that results in unfair or inaccurate predictions for certain subgroups. It often originates from unrepresentative training data.
- Deep Learning: A subfield of machine learning based on artificial neural networks with many layers, particularly effective for pattern recognition in complex data like images.
- Explainability (XAI): Methods and techniques that enable human users to understand and trust the results and output created by machine learning algorithms.
- Machine Learning: A type of AI that provides computers with the ability to learn from data without being explicitly programmed.
For a global perspective on policy and ethics, the World Health Organization’s page on AI for health is an excellent resource for policymakers and administrators.