A Practitioner’s Guide to Artificial Intelligence in Healthcare: From Implementation to Outcomes
Table of Contents
- Executive summary
- The state of AI in healthcare today
- Clinical applications reshaping care
- Data, interoperability and quality challenges
- Model evaluation, validation and benchmarking
- Regulatory, ethical and equity considerations
- Implementation roadmap for health systems
- Measuring patient outcomes and value
- Security and risk mitigation strategies
- Short anonymized case vignettes
- Deployment checklist: 12 essential steps
- Further reading and references
Executive summary
The integration of Artificial Intelligence in Healthcare has moved from theoretical potential to practical application, offering transformative capabilities in diagnostics, treatment personalization, and operational efficiency. This guide is designed for clinicians, health system leaders, and data scientists navigating this complex landscape. It provides a practitioner-focused overview of core AI technologies, their clinical applications, and the critical challenges of data governance, model validation, and regulatory compliance. By focusing on a structured implementation roadmap, measurable clinical outcomes, and robust ethical safeguards, this article serves as a blueprint for successfully deploying AI solutions to improve patient care and create tangible value within health systems.
The state of AI in healthcare today
The conversation around Artificial Intelligence in Healthcare has matured significantly. We are moving beyond the initial hype cycle into a phase of tangible, evidence-based implementation. While foundational research continues to push boundaries, the focus for health systems is now on integrating validated AI tools into existing clinical workflows to address specific, high-impact problems. This shift is driven by the increasing availability of digitized health data, advancements in computational power, and the development of more sophisticated algorithms. The challenge is no longer just about building a predictive model; it’s about deploying it safely, ethically, and in a way that demonstrably improves patient outcomes and clinician experience.
Core technologies explained: machine learning, deep learning, natural language processing, reinforcement learning
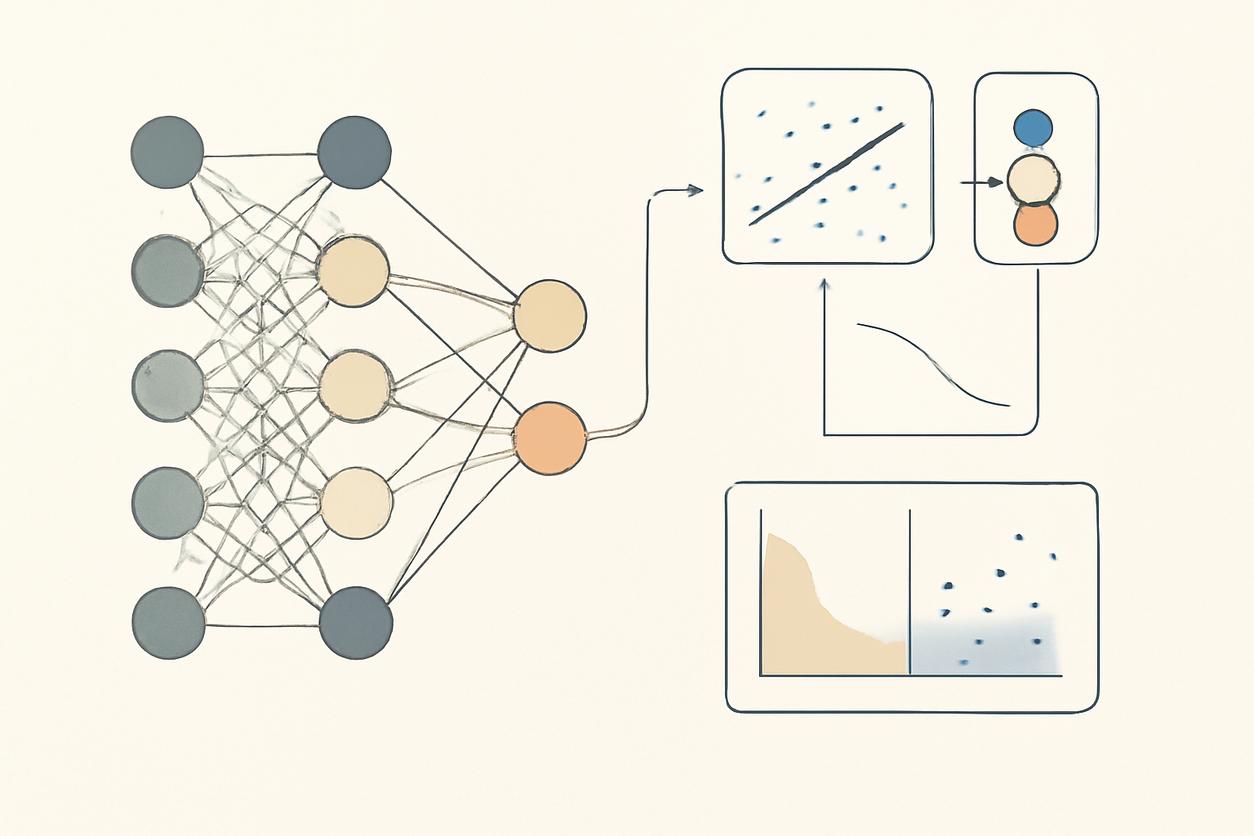
Understanding the core technologies is essential for any discussion of Artificial Intelligence in Healthcare. These are not monolithic concepts but a suite of tools, each suited for different clinical challenges.
- Machine Learning (ML): This is the foundational field of AI where algorithms are trained on data to identify patterns and make predictions without being explicitly programmed. In a clinical context, an ML model could analyze electronic health record (EHR) data to predict a patient’s risk of developing sepsis.
- Deep Learning (DL): A specialized subset of ML, deep learning uses complex, multi-layered neural networks to analyze highly intricate data. It has proven exceptionally powerful in medical imaging, where DL models can detect subtle patterns in X-rays, CT scans, or pathology slides that may be invisible to the human eye.
- Natural Language Processing (NLP): NLP gives computers the ability to understand and interpret human language. In healthcare, this is critical for unlocking the vast amount of unstructured data trapped in clinical notes, physician dictations, and patient communications, enabling applications like clinical trial matching and sentiment analysis.
- Reinforcement Learning (RL): This advanced technique involves training an AI “agent” to make a sequence of decisions to maximize a cumulative reward. While still emerging in clinical practice, its potential applications include optimizing dynamic treatment regimens for chronic diseases or managing hospital resource allocation in real-time.
Clinical applications reshaping care
The true value of Artificial Intelligence in Healthcare is realized through its application at the point of care. Across various specialties, AI is augmenting clinical capabilities and streamlining complex processes.
Diagnostics and imaging
Medical imaging is one of the most mature domains for AI application. Deep learning algorithms are now capable of analyzing radiological images—such as mammograms for breast cancer, chest X-rays for pneumonia, and brain MRIs for strokes—with accuracy that can meet or even exceed human performance. These tools act as a “second reader” for radiologists, helping to prioritize critical cases, reduce diagnostic errors, and improve the overall efficiency of the imaging workflow.
Triage and clinical decision support
In high-pressure environments like the emergency department, AI-powered triage tools can help clinicians prioritize patients by predicting the likelihood of critical illness based on initial vital signs and chief complaints. Furthermore, clinical decision support systems (CDSS) integrated into the EHR can alert providers to potential drug interactions, suggest differential diagnoses based on patient data, and surface relevant clinical guidelines, all within the existing workflow.
Treatment planning and predictive monitoring
AI is enabling a new era of personalized medicine. In oncology, for instance, algorithms can analyze genomic data, imaging, and pathology reports to recommend tailored treatment plans. In the intensive care unit (ICU), predictive models continuously monitor streams of physiological data to provide early warnings of patient deterioration, allowing for proactive intervention before a crisis occurs. This shift from reactive to predictive care is a cornerstone of modern healthcare AI.
Data, interoperability and quality challenges
The performance of any AI model is fundamentally limited by the quality and accessibility of the data it is trained on. Healthcare data is notoriously complex, existing in fragmented silos across different systems and formats. Achieving interoperability—the seamless exchange of data between systems—is a primary challenge. Furthermore, issues of data quality, including missing values, inconsistent labeling, and inherent biases, must be rigorously addressed before any model development can begin. A successful Artificial Intelligence in Healthcare strategy is built on a foundation of clean, standardized, and representative data.
Data governance and privacy
Robust data governance is non-negotiable. This involves establishing clear policies and procedures for how data is collected, stored, accessed, and used. Patient privacy must be paramount, with strict adherence to regulations like the Health Insurance Portability and Accountability Act (HIPAA) in the United States. Techniques such as data de-identification, anonymization, and the use of secure, federated learning environments are critical for developing AI models while protecting sensitive patient information.
Model evaluation, validation and benchmarking
A model that performs well on a training dataset does not guarantee clinical utility. Rigorous evaluation and validation are essential steps to ensure an AI tool is safe and effective.
- Internal Validation: Testing the model on a holdout set of data from the same institution where it was developed. This is a crucial first step but is insufficient on its own.
- External Validation: Testing the model on data from different institutions, patient populations, and clinical settings. This step is critical for assessing the model’s generalizability and robustness.
- Clinical Validation: Ideally conducted through a prospective, randomized controlled trial, this step evaluates the model’s real-world impact on clinical workflows, decision-making, and patient outcomes.
Benchmarking against existing clinical standards and other AI models provides necessary context for performance and helps health systems make informed procurement and deployment decisions.
Regulatory, ethical and equity considerations
As AI becomes more integrated into clinical practice, regulatory and ethical oversight becomes increasingly important. In the U.S., the Food and Drug Administration (FDA) regulates many AI tools as Software as a Medical Device (SaMD), requiring evidence of safety and effectiveness. Beyond regulation, health systems must grapple with profound ethical questions. How do we ensure AI models are fair and do not perpetuate or amplify existing health disparities? Who is accountable when an AI model contributes to a poor patient outcome? Ensuring transparency and explainability—the ability to understand why a model made a particular prediction—is key to building trust with clinicians and patients.
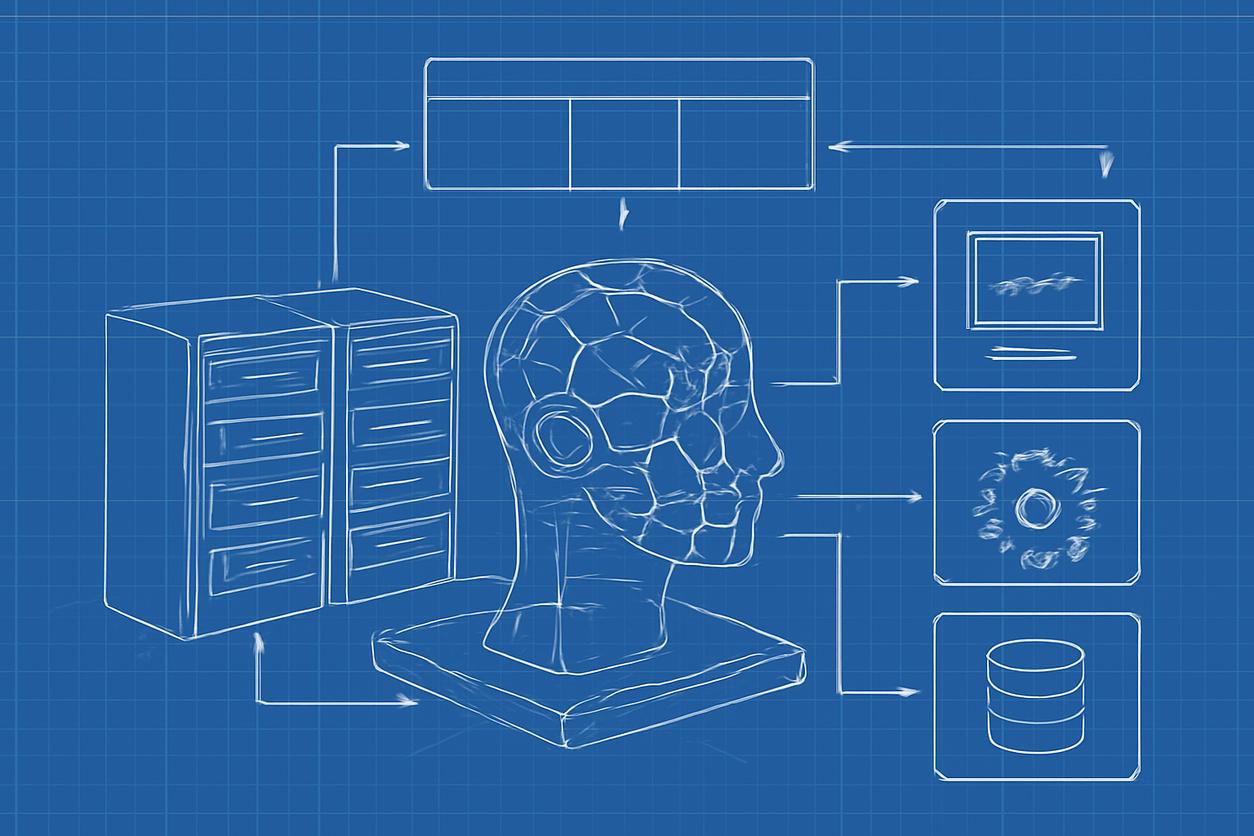
Implementation roadmap for health systems
A structured, phased approach is critical for successfully implementing Artificial Intelligence in Healthcare. This roadmap moves from a controlled pilot to full-scale operationalization.
Pilot design and stakeholder alignment
The journey should begin with a well-defined clinical pilot focused on a specific, measurable problem. Success requires strong stakeholder alignment from the outset, bringing together a cross-functional team of clinicians, IT specialists, data scientists, and administrative leaders. Clear success metrics—both clinical and operational—must be established before the pilot begins to ensure its impact can be objectively evaluated.
Scaling and operationalizing models
Moving from a successful pilot to an enterprise-wide solution presents a new set of challenges. This phase requires deep integration with existing clinical workflows, most notably the EHR. Significant resources must be dedicated to end-user training and support to ensure clinicians can use the tool effectively and trust its outputs. Furthermore, a plan for continuous monitoring is essential to track model performance over time and detect “model drift,” where performance degrades as patient populations or clinical practices change.
Measuring patient outcomes and value
The ultimate measure of any healthcare AI tool is its impact on patient care. While technical metrics like accuracy are important for development, the true value is demonstrated through improvements in clinical outcomes. Health systems must track metrics such as:
- Reductions in patient mortality or morbidity
- Decreased hospital length of stay
- Lower readmission rates
- Improved patient safety indicators
- Enhanced patient satisfaction
Quantifying this value is essential for building a business case for continued investment in Artificial Intelligence in Healthcare and demonstrating a tangible return on investment.
Security and risk mitigation strategies
AI systems introduce new cybersecurity vulnerabilities. Adversarial attacks, where malicious actors introduce intentionally crafted data to fool a model, pose a significant risk, particularly in diagnostics. Data poisoning during the training phase can also compromise a model’s integrity. Mitigation strategies for 2025 and beyond will focus on building robust, resilient AI systems, implementing continuous anomaly detection, and adopting a zero-trust security framework for all data pipelines and model interfaces involved in the AI lifecycle.
Short anonymized case vignettes
Vignette 1: Sepsis Prediction in the ICU. A large academic medical center deployed an EHR-integrated ML model to predict sepsis onset in ICU patients. The model continuously analyzed over 50 variables, providing a risk score updated every hour. A “silent alert” was sent to a dedicated nursing team for high-risk patients, prompting a standardized protocol review. A post-implementation analysis showed a 15% relative reduction in sepsis-related mortality and a half-day reduction in average ICU length of stay for septic patients.
Vignette 2: Streamlining Radiology Workflows. A community hospital network implemented a deep learning tool to screen all outpatient chest X-rays for critical findings like pneumothorax and nodules. The system automatically flagged suspicious studies and moved them to the top of the radiologist’s worklist. This reduced the median report turnaround time for critical findings from four hours to under 30 minutes, enabling faster patient follow-up.
Deployment checklist: 12 essential steps
Use this checklist as a high-level guide for any clinical AI implementation project.
- Define the Clinical Problem: Identify a specific, high-value clinical challenge that AI can address.
- Assemble a Cross-Functional Team: Include clinicians, IT, data scientists, ethics, and leadership.
- Assess Data Readiness and Governance: Ensure access to high-quality, representative data and have clear governance policies.
- Select or Develop an Appropriate Model: Choose the right AI technique for the problem; decide whether to build, buy, or partner.
- Conduct Rigorous Internal Validation: Test the model extensively on local, held-out data.
- Perform External and Clinical Validation: Validate the model on diverse datasets and, if possible, in a prospective clinical study.
- Address Regulatory and Ethical Requirements: Secure necessary regulatory clearance and conduct a thorough ethical and bias review.
- Design a Limited Clinical Pilot: Test the model in a controlled environment with a small group of end-users.
- Integrate with Clinical Workflows: Ensure the tool is seamlessly embedded in the clinician’s daily workflow (e.g., EHR).
- Train End-Users Thoroughly: Provide comprehensive training on how the tool works, its limitations, and its role in decision-making.
- Monitor Model Performance Post-Deployment: Continuously track model accuracy, drift, and usage.
- Measure Clinical and Economic Impact: Evaluate the project against the pre-defined outcome and value metrics.
Further reading and references
For those seeking to deepen their understanding of Artificial Intelligence in Healthcare, the following resources provide access to cutting-edge research, policy guidelines, and public health perspectives.
- PubMed: A comprehensive database of biomedical literature for peer-reviewed research on clinical AI validation and outcomes.
- National Institutes of Health (NIH): A primary source for funded research initiatives and strategic plans related to AI in medicine.
- World Health Organization (WHO): Provides a global perspective on the ethics and governance of AI for health.
- arXiv: A repository for pre-print research articles, offering early access to the latest technical advancements in machine learning.
- U.S. Food and Drug Administration (FDA): The definitive resource for regulatory guidance on AI and machine learning-enabled medical devices.