Table of Contents
- Executive Summary
- Why Artificial Intelligence Now in Clinical Care
- Core AI Approaches and Where They Fit in Medicine
- Case Study: Diagnostic Imaging Workflow
- Case Study: Predictive Patient Monitoring
- Data Curation, Labeling and Quality Requirements
- Model Validation, Evaluation and Clinical Trials
- Governance, Ethics and Bias Mitigation Strategies
- Integration with Electronic Health Records and Interoperability
- Security, Privacy and Data Minimization Practices
- Operational Deployment Pathways and Change Management
- Measuring Clinical Impact and Continuous Learning
- Barriers, Risks and Practical Mitigations
- Regulatory Landscape and Compliance Considerations
- Pilot Project Checklist and Timeline
- Further Reading and Curated Resources
Executive Summary
The integration of Artificial Intelligence in Healthcare represents a paradigm shift, moving the industry from a reactive to a predictive and personalized model of care. This whitepaper serves as a practical roadmap for healthcare leaders, clinicians, and IT managers navigating this transformation. We explore the confluence of factors accelerating AI adoption, from vast data availability to mature algorithmic capabilities. This document demystifies core AI techniques—machine learning, natural language processing, and computer vision—by grounding them in concrete clinical workflows, such as diagnostic imaging and predictive patient monitoring. We provide a comprehensive framework covering the entire AI lifecycle, from data curation and model validation to ethical governance, EHR integration, and regulatory compliance. The unique focus is on actionable strategies and measurable outcomes, offering a pragmatic guide to harnessing the power of Artificial Intelligence in Healthcare to enhance patient outcomes, improve operational efficiency, and drive the future of medicine.
Why Artificial Intelligence Now in Clinical Care
The current momentum behind Artificial Intelligence in Healthcare is not a sudden event but the culmination of several converging trends. Healthcare systems are generating data at an unprecedented rate, fueled by the widespread adoption of electronic health records (EHRs), genomic sequencing, wearable devices, and advanced medical imaging. This data deluge, while overwhelming for human analysis, provides the raw material for sophisticated AI models.
Simultaneously, advancements in computational power, particularly the development of Graphics Processing Units (GPUs), have made it feasible to train complex deep learning models that were once computationally prohibitive. This technological maturity allows AI to move beyond academic research and into practical clinical applications. The imperative to improve efficiency, manage rising costs, and address challenges like clinician burnout further intensifies the need for intelligent tools that can augment human expertise, automate routine tasks, and uncover insights hidden within complex datasets.
Core AI Approaches and Where They Fit in Medicine
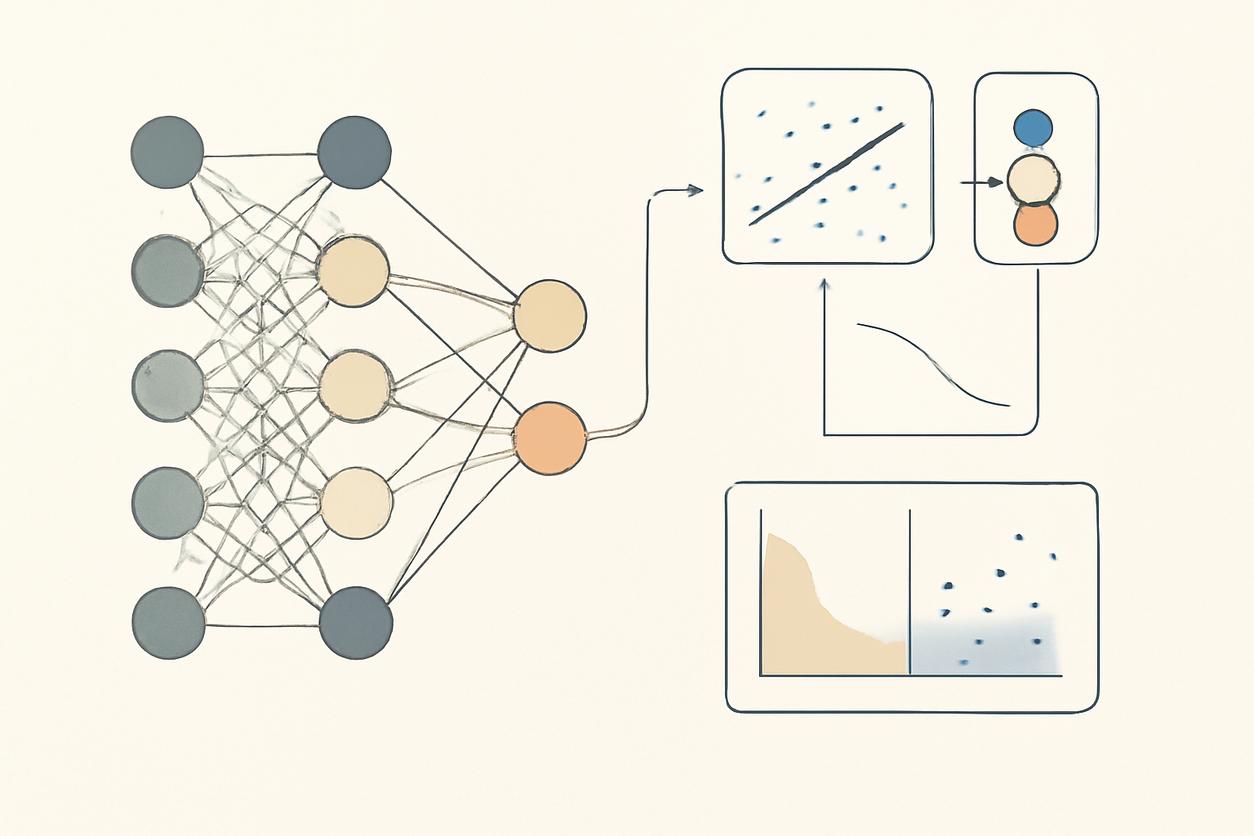
Understanding the fundamental types of AI is crucial for identifying appropriate use cases. The field of Artificial Intelligence in Healthcare primarily leverages three core methodologies.
Machine Learning (ML)
Machine Learning is a subset of AI where algorithms learn patterns from data without being explicitly programmed. Key types include:
- Supervised Learning: The model is trained on labeled data (e.g., patient records with known outcomes) to make predictions. Applications include predicting patient readmission risk or identifying cancerous cells in a biopsy image.
- Unsupervised Learning: The model identifies hidden patterns in unlabeled data. This is useful for patient stratification, identifying distinct patient subgroups with similar characteristics for personalized treatment plans.
- Reinforcement Learning: The model learns through trial and error, receiving rewards or penalties for its actions. It has potential in optimizing dynamic treatment regimens for chronic diseases.
Natural Language Processing (NLP)
A significant portion of valuable clinical information is locked in unstructured text, such as physician notes, discharge summaries, and pathology reports. NLP enables computers to understand, interpret, and generate human language. In healthcare, it is used to extract structured data from clinical notes, power clinical documentation improvement tools, and analyze patient sentiment from feedback.
Computer Vision
Computer vision allows AI models to interpret and analyze visual information from the world, particularly medical images. This has been one of the most impactful areas of Artificial Intelligence in Healthcare to date, with applications in:
- Radiology: Detecting nodules in CT scans or fractures in X-rays.
- Pathology: Identifying and grading tumors in digital pathology slides.
- Dermatology: Classifying skin lesions from photographs.
Case Study: Diagnostic Imaging Workflow
Consider the integration of an AI model into a standard radiology workflow for chest X-rays. The goal is to improve accuracy and reduce turnaround time.
- Image Acquisition and Triage: As a chest X-ray is acquired, the AI model automatically analyzes it in seconds. It flags images with a high probability of critical findings (e.g., pneumothorax) and moves them to the top of the radiologist’s worklist.
- Augmented Reading: The radiologist opens the study. The AI has already overlaid a “heat map” highlighting suspicious areas and may provide preliminary measurements or classifications. This acts as a second reader, drawing attention to subtle findings that might be missed.
- Report Generation: The radiologist confirms or rejects the AI’s findings. NLP tools can then assist by auto-populating sections of the radiology report based on the confirmed findings, saving significant documentation time.
This workflow does not replace the radiologist but augments their capabilities, allowing them to focus their expertise on complex cases and final validation, thereby increasing throughput and diagnostic confidence.
Case Study: Predictive Patient Monitoring
In an Intensive Care Unit (ICU), a predictive AI model can be a life-saving tool for early detection of patient deterioration, such as the onset of sepsis.
- Real-Time Data Ingestion: The AI model continuously ingests multiple streams of real-time data from the patient’s bedside monitor (heart rate, blood pressure, oxygen saturation) and the EHR (lab results, medications).
- Pattern Recognition: The model has been trained on thousands of previous ICU patient records to recognize the subtle, complex patterns that often precede a sepsis event, often hours before clinical signs become obvious.
- Alerting and Intervention: When the model’s risk score for a patient crosses a predefined threshold, it sends a non-intrusive alert to the clinical team’s dashboard. The alert includes the patient’s risk score and the key contributing factors (e.g., rising lactate, slight drop in blood pressure), prompting a timely bedside evaluation and potential early intervention.
This application of Artificial Intelligence in Healthcare shifts the care paradigm from reacting to a crisis to proactively preventing it, leading to better patient outcomes and reduced length of stay.
Data Curation, Labeling and Quality Requirements
The performance of any AI model is fundamentally limited by the quality of the data it is trained on. The principle of “garbage in, garbage out” is paramount. For successful implementation of Artificial Intelligence in Healthcare, organizations must invest in robust data infrastructure and governance.
Key Requirements:
- Data Quality: Data must be accurate, complete, and consistent. This involves addressing issues like missing values, incorrect entries, and inconsistent formatting across different data sources.
- Data Labeling: For supervised learning, data must be accurately labeled by subject matter experts. For example, medical images must be annotated by experienced radiologists. This is often the most time-consuming and expensive part of model development.
- Data Diversity and Representativeness: The training data must reflect the diversity of the patient population on which the model will be used. A lack of diversity can lead to significant performance gaps and algorithmic bias.
Model Validation, Evaluation and Clinical Trials
A model that performs well in a lab environment may fail in a real-world clinical setting. Rigorous validation is non-negotiable.
Validation Stages:
- Internal Validation: The model is tested on a holdout set of data from the same source it was trained on. This is a first check for performance using metrics like accuracy, precision, recall, and AUC-ROC.
- External Validation: The model is tested on entirely new datasets from different institutions, patient populations, or equipment vendors. This is crucial for assessing its generalizability and robustness.
- Clinical Trials: The gold standard is a prospective, randomized controlled trial to evaluate the AI tool’s impact on clinical outcomes, workflow efficiency, and patient safety in a live clinical environment. This step is often required for regulatory approval.
Governance, Ethics and Bias Mitigation Strategies
As Artificial Intelligence in Healthcare becomes more autonomous, establishing strong governance and ethical frameworks is essential to build trust and ensure patient safety.
Mitigation Strategies for 2025 and Beyond:
- Establish an AI Governance Committee: A multidisciplinary committee including clinicians, data scientists, ethicists, and patient representatives should oversee the development, validation, and deployment of all AI tools.
- Conduct Algorithmic Bias Audits: Before deployment, models must be systematically audited for performance disparities across different demographic groups (e.g., race, gender, age). The goal is to identify and mitigate biases inherited from historical data.
- Prioritize Explainable AI (XAI): For high-stakes decisions, “black box” models are often unacceptable. Invest in XAI techniques that can provide clinicians with a rationale for the AI’s output, fostering trust and enabling them to override incorrect suggestions.
- Human-in-the-Loop Design: Ensure that a qualified clinician is always in a position to oversee, interpret, and make the final decision based on an AI model’s recommendation, especially in diagnostic and treatment contexts.
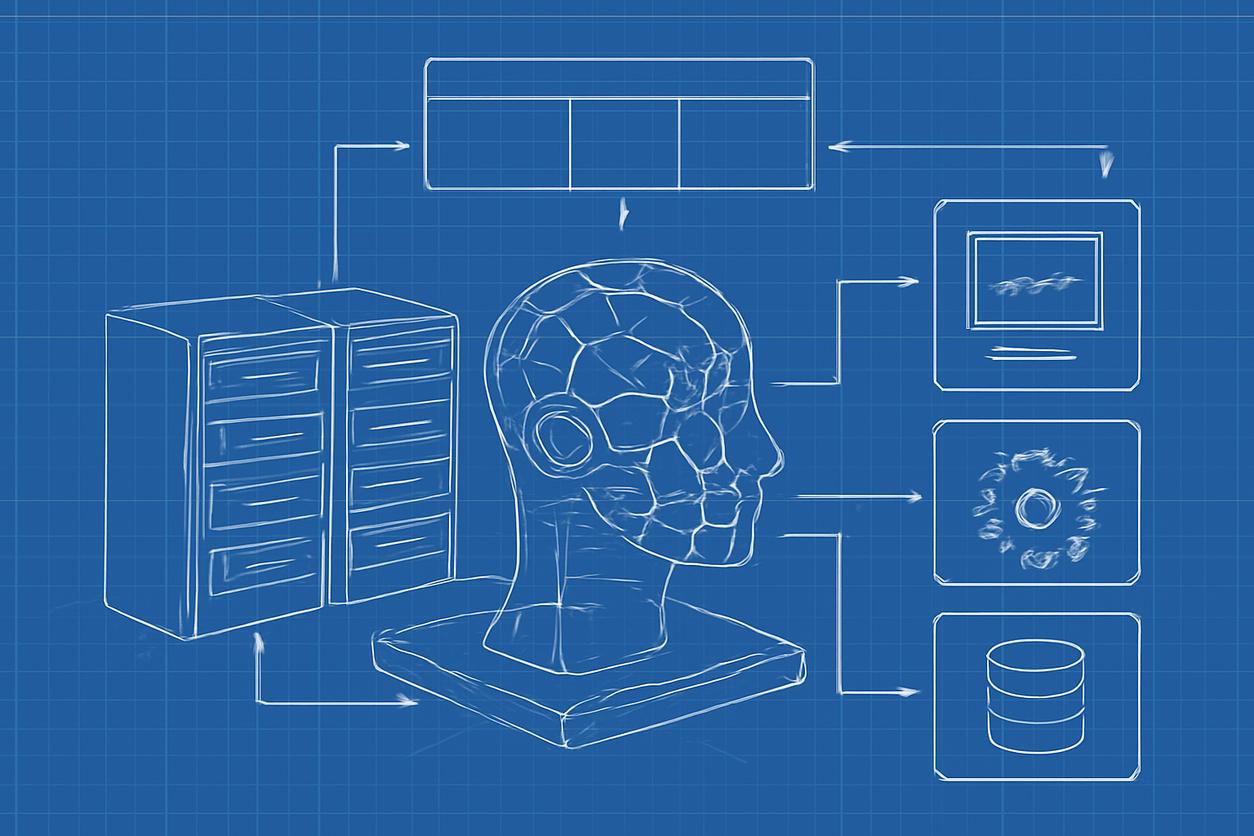
Integration with Electronic Health Records and Interoperability
For an AI tool to be useful, it must integrate seamlessly into existing clinical workflows, which are typically centered around the EHR. Poor integration leads to user frustration and low adoption.
Key Considerations:
- Interoperability Standards: Leverage modern standards like FHIR (Fast Healthcare Interoperability Resources) to enable smooth, real-time data exchange between the AI application and the EHR system. This avoids manual data entry and information silos.
- Workflow-Native Design: The AI’s outputs and insights should be presented directly within the clinician’s existing EHR interface, not in a separate, standalone application. This minimizes clicks and context switching.
Security, Privacy and Data Minimization Practices
Patient data is highly sensitive, and its use in AI systems must adhere to strict security and privacy protocols like HIPAA in the United States.
Best Practices:
- Data Minimization: The AI model should only be trained and run on the minimum amount of data necessary to perform its function. Avoid using extraneous patient identifiers or protected health information (PHI) if not required.
- Federated Learning: This emerging technique allows an AI model to be trained across multiple institutions without the patient data ever leaving its source hospital’s firewall. A central model is updated with learnings from each site, enhancing privacy.
- Robust Cybersecurity: Implement strong access controls, encryption of data at rest and in transit, and regular security audits to protect the AI system and its data from breaches.
Operational Deployment Pathways and Change Management
The successful deployment of Artificial Intelligence in Healthcare is as much a change management challenge as it is a technical one.
Phased Rollout Strategy:
- Silent Mode: Initially, run the AI model in the background without displaying its results to clinicians. This allows for performance monitoring in a real-world setting without affecting clinical care.
- Limited Pilot: Deploy the tool to a small group of champion users who can provide valuable feedback for workflow refinement.
- Broad Rollout: After successful piloting, roll the tool out to the wider organization, accompanied by comprehensive training, clear documentation, and ongoing support.
Measuring Clinical Impact and Continuous Learning
To justify the investment in AI, its impact must be measured against predefined key performance indicators (KPIs). These should cover clinical, operational, and financial domains.
| Domain | Example KPIs |
|---|---|
| Clinical Outcomes | Improved diagnostic accuracy, reduced mortality rates, lower complication rates. |
| Operational Efficiency | Reduced report turnaround time, decreased patient length of stay, optimized resource allocation. |
| Financial Impact | Lower readmission penalties, reduced cost of care per patient, increased throughput. |
Furthermore, AI models are not static. A framework for continuous learning must be in place to monitor for model drift (performance degradation over time) and to retrain the model with new data to maintain its accuracy and relevance.
Barriers, Risks and Practical Mitigations
Deploying Artificial Intelligence in Healthcare is not without its challenges. Proactive identification and mitigation are key.
- Barrier: Poor Data Quality. Mitigation: Invest in data governance and a dedicated data curation team. Start with a well-defined, high-quality dataset for a specific use case.
- Risk: Algorithmic Bias. Mitigation: Implement fairness audits and ensure training data is representative of the target population. Use XAI to understand model behavior.
- Barrier: Clinician Resistance. Mitigation: Involve clinicians from the very beginning of the project. Focus on AI as an augmentation tool, not a replacement. Provide thorough training and support.
- Risk: The “Black Box” Problem. Mitigation: Prioritize interpretable models where possible. For complex models, use XAI tools to provide insight into decision-making.
Regulatory Landscape and Compliance Considerations
AI in healthcare is regulated medical technology. In the U.S., the U.S. Food and Drug Administration (FDA) oversees many of these tools under its “Software as a Medical Device” (SaMD) framework. The regulatory landscape is evolving rapidly to keep pace with technology. Organizations must stay informed about clearance and approval pathways and maintain meticulous documentation of their model’s development, validation, and post-market surveillance processes to ensure compliance.
Pilot Project Checklist and Timeline
A structured approach is critical for a successful first AI project.
Checklist for a Pilot Project (Starting in 2025):
- Define a Clear, High-Impact Problem: Identify a specific clinical or operational challenge where AI can provide significant value.
- Assemble a Multidisciplinary Team: Include clinicians, data scientists, IT staff, and an executive sponsor.
- Assess Data Availability and Quality: Confirm you have access to a sufficient volume of high-quality, relevant data.
- Select a Vendor or Develop In-House: Evaluate whether to partner with a specialized AI vendor or build the capability internally.
- Establish Success Metrics: Define the clinical and operational KPIs you will use to measure the pilot’s success.
- Plan for Workflow Integration: Map out exactly how the AI tool will fit into the existing clinical workflow.
- Obtain Ethical and Governance Approval: Ensure the project is reviewed and approved by your organization’s governance committee.
High-Level Timeline (Example):
- Q1 2025: Problem identification and team assembly.
- Q2 2025: Data access, curation, and initial model development/vendor selection.
- Q3 2025: Model validation, workflow integration planning, and governance approval.
- Q4 2025: Deployment of pilot in “silent mode” or to a limited user group.
- Q1 2026: Evaluation of pilot results against predefined KPIs and decision on broader rollout.
Further Reading and Curated Resources
The field of Artificial Intelligence in Healthcare is dynamic. Staying informed is essential for all stakeholders. The following resources provide authoritative information, research, and guidelines:
- World Health Organization: Provides global guidance on the ethics and governance of artificial intelligence for health.
- National Institutes of Health: Funds and conducts extensive research on the application of AI and data science in biomedical research and healthcare.
- Partnership on AI: A multi-stakeholder organization that develops best practices and public guidance on AI technologies to benefit people and society.
- Nature Medicine: A leading peer-reviewed journal that frequently publishes cutting-edge research and commentary on the clinical application and validation of AI in medicine.