The Clinical Co-Pilot: A Leader’s Guide to Artificial Intelligence in Healthcare
This paper serves as a strategic overview of the applications, challenges, and opportunities presented by the integration of Artificial Intelligence in Healthcare. It is designed for clinical leaders, technology innovators, and policy advisors navigating this transformative landscape.
Table of Contents
- Executive snapshot: Why this matters now
- Foundations: Neural networks, deep learning and reinforcement learning
- Language at scale: NLP for clinical text and patient communication
- Seeing beneath the surface: Deep learning for medical imaging
- Predictive pathways: Risk stratification and clinical decision support
- Operational intelligence: Scheduling, supply and resource prediction
- Safety by design: Responsible AI and governance checkpoints
- Data stewardship and security considerations
- Deployment blueprint: Pilots, validation and scaling
- Measuring success: Clinical outcomes, cost and adoption metrics
- Barriers and common misconceptions
- Forward view: Autonomous systems and cognitive augmentation
- Appendix: Glossary, methodology and curated readings
Executive snapshot: Why this matters now
The convergence of unprecedented data availability, exponential growth in computational power, and sophisticated algorithmic innovation has propelled Artificial Intelligence in Healthcare from a theoretical concept to a practical clinical tool. Healthcare systems globally face immense pressure from rising costs, aging populations, and workforce shortages. AI offers not a replacement for human expertise, but an augmentation—a “clinical co-pilot” capable of analyzing vast datasets to uncover insights, streamline operations, and support evidence-based decision-making at a scale previously unimaginable. This transition requires more than technological adoption; it demands strategic vision, ethical governance, and a commitment to transforming clinical workflows to deliver safer, more efficient, and personalized patient care.
Foundations: Neural networks, deep learning and reinforcement learning
Understanding the core technologies behind Artificial Intelligence in Healthcare is essential for effective leadership and implementation. These systems are not magic; they are advanced computational models designed to learn from data.
Core Concepts in Clinical AI
- Artificial Neural Networks (ANNs): Inspired by the structure of the human brain, ANNs are computing systems comprised of interconnected nodes, or “neurons.” They form the foundation of most modern AI, processing data in layers to recognize patterns. In a clinical context, an ANN might learn to identify correlations between patient lab results and specific conditions.
- Deep Learning (DL): This is a subfield of machine learning based on ANNs with many layers (hence “deep”). Deep learning excels at identifying intricate patterns in large, complex datasets like medical images, genomic sequences, or electronic health records (EHRs). Its ability to learn features automatically makes it a powerful tool for diagnostic support.
- Reinforcement Learning (RL): Where deep learning is adept at perception, reinforcement learning is focused on decision-making. An RL agent learns to achieve a goal in a complex, uncertain environment by taking actions and observing the outcomes (rewards or penalties). Potential healthcare applications include optimizing treatment protocols or managing hospital resource allocation dynamically.
Language at scale: NLP for clinical text and patient communication
A significant portion of critical patient information—up to 80%—is locked away in unstructured formats like clinician notes, pathology reports, and patient correspondence. Natural Language Processing (NLP) is the branch of AI that gives computers the ability to understand, interpret, and generate human language, unlocking this vital data source.
Key NLP Applications
- Clinical Documentation Improvement (CDI): NLP algorithms can scan EHR notes in real-time to suggest more specific diagnostic codes, improving billing accuracy and data quality for research.
- Data De-identification: To facilitate research and data sharing, NLP can automatically remove Protected Health Information (PHI) from clinical texts, mitigating privacy risks.
- Cohort Identification: Researchers can use NLP to rapidly search millions of clinical records to identify patient cohorts for clinical trials based on specific narrative criteria, drastically accelerating recruitment.
- Sentiment Analysis: By analyzing patient feedback from surveys or digital communications, healthcare systems can gain real-time insights into patient experience and satisfaction.
Seeing beneath the surface: Deep learning for medical imaging
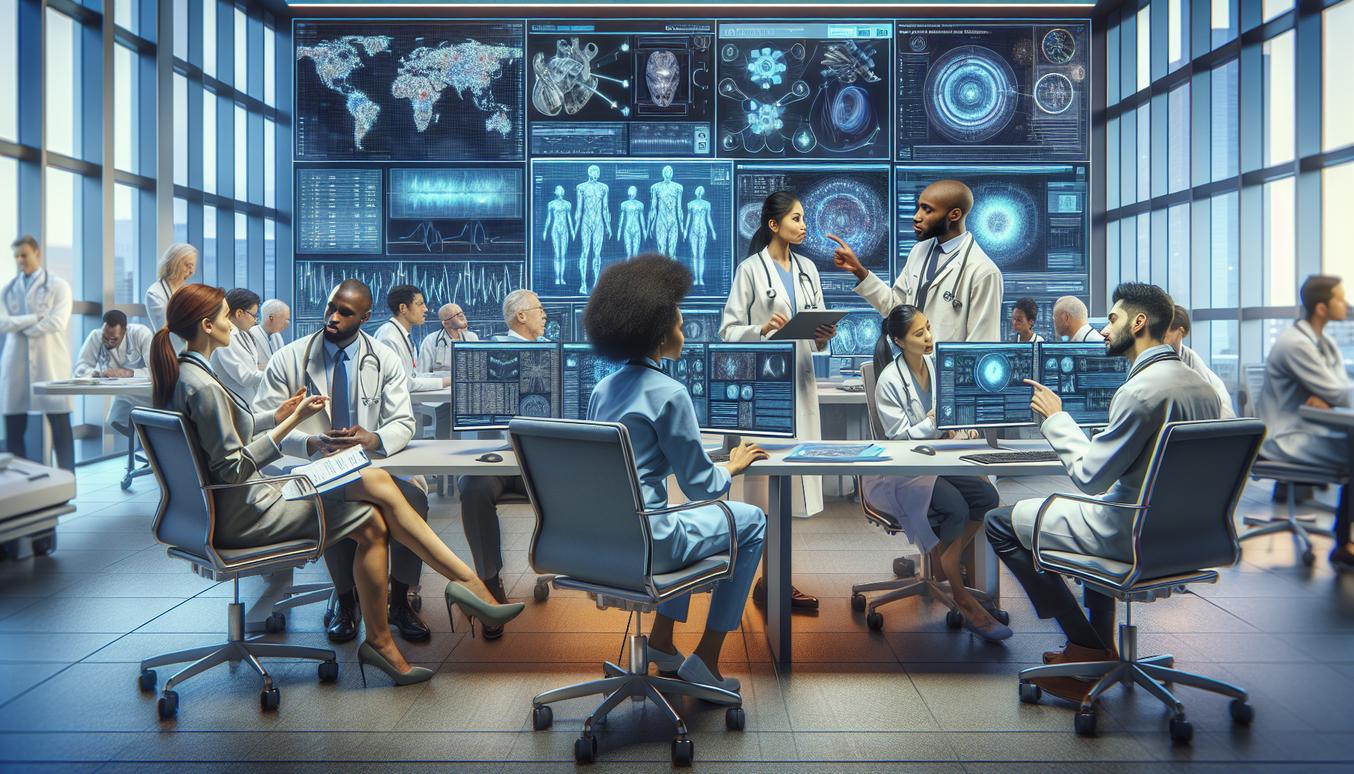
Medical imaging is one of the most mature domains for the application of Artificial Intelligence in Healthcare. Deep learning models, particularly Convolutional Neural Networks (CNNs), have demonstrated performance on par with, and in some cases exceeding, human experts in specific diagnostic tasks.
Transforming Diagnostics with AI
The field of Deep Learning in Medical Imaging is rapidly advancing across multiple specialities:
- Radiology: AI algorithms can triage scans by flagging suspected abnormalities (e.g., nodules in a chest X-ray, hemorrhages in a brain CT) for priority review, reducing turnaround times for critical findings.
- Pathology: Analyzing digital pathology slides, AI can assist in cancer grading by quantifying mitotic counts or identifying metastatic cells, improving consistency and reducing pathologist workload.
- Dermatology: Image analysis models trained on thousands of dermatoscopic images can help classify skin lesions and assist in the early detection of melanomas.
- Ophthalmology: AI tools can screen retinal fundus images for signs of diabetic retinopathy or macular degeneration, enabling earlier intervention and prevention of vision loss.
Predictive pathways: Risk stratification and clinical decision support
Beyond identifying existing disease, a core promise of Artificial Intelligence in Healthcare is its ability to forecast future events. By analyzing thousands of variables within an EHR, Predictive Modelling can provide clinicians with crucial foresight.
From Reactive to Proactive Care
- Sepsis Prediction: Early warning systems can continuously monitor vital signs, lab results, and clinical notes to predict the onset of sepsis hours before it becomes clinically apparent, allowing for life-saving early intervention.
- Readmission Risk: Models can identify patients at high risk of hospital readmission upon discharge, enabling care teams to allocate transitional care resources more effectively.
- Deterioration Forecasting: On general hospital wards, AI can provide a continuous risk score for patient deterioration, helping to prioritize nursing attention and prevent “failure to rescue” events.
- Personalized Treatment Response: By analyzing a patient’s genomic, clinical, and lifestyle data, predictive models can help forecast which treatment protocol is most likely to be effective for that individual.
Operational intelligence: Scheduling, supply and resource prediction
The impact of AI extends beyond direct patient care to the core operational efficiency of healthcare organizations. By optimizing logistics and resource management, AI can reduce costs, decrease patient wait times, and improve staff satisfaction.
Building a Smarter Hospital
- Operating Room Scheduling: AI can optimize surgical schedules by predicting procedure durations more accurately and accounting for variables like surgeon availability and equipment needs, maximizing throughput.
- Staffing and Roster Management: Predictive models can forecast patient admission volumes and acuity, allowing for more efficient and proactive staff scheduling to prevent understaffing or overstaffing.
- Supply Chain Optimization: By predicting the demand for medications, personal protective equipment (PPE), and other critical supplies, AI can help prevent stockouts and reduce waste.
Safety by design: Responsible AI and governance checkpoints
The power of Artificial Intelligence in Healthcare comes with profound responsibility. A proactive approach to ethics and governance is not optional but essential for building trust and ensuring patient safety. Organizations must establish robust Responsible AI Frameworks.
Core Pillars of Ethical AI
- Fairness and Bias Mitigation: AI models trained on historical data can perpetuate and even amplify existing biases. It is critical to audit datasets for representation and test models for performance equity across different demographic groups.
- Transparency and Interpretability: Clinicians must have a degree of insight into why an AI model makes a particular recommendation. While not all models can be fully transparent (“white box”), techniques for interpretability (“explainable AI”) are crucial for clinical acceptance.
- Accountability and Oversight: Clear lines of accountability must be established. Who is responsible when an AI system contributes to an adverse event? Governance structures must include “human-in-the-loop” validation for high-stakes decisions.
- Robustness and Reliability: Models must be rigorously tested against adversarial attacks and data drift to ensure they perform reliably and safely when deployed in real-world clinical environments.
Data stewardship and security considerations
Data is the lifeblood of any AI system. The success of any initiative for Artificial Intelligence in Healthcare is contingent upon a robust data strategy that prioritizes quality, security, and privacy.
Prerequisites for Effective AI
- Data Quality: The “garbage in, garbage out” principle applies. AI models are only as good as the data they are trained on. This requires investment in data cleaning, standardization, and interoperability.
- Security and Privacy: Patient data must be protected with state-of-the-art security measures. Techniques like federated learning, where models are trained locally without centralizing sensitive data, and robust de-identification are key to preserving privacy.
- Regulatory Compliance: All AI activities must adhere to regulations such as HIPAA in the United States or GDPR in Europe, ensuring patient consent and data rights are respected.
Deployment blueprint: Pilots, validation and scaling
Moving an AI model from a research environment to a live clinical workflow is a complex undertaking. A phased, evidence-based approach is critical for success.
A Strategic Rollout Plan
- Problem Selection: Begin with a well-defined, high-impact clinical or operational problem where the data and infrastructure exist to support an AI solution.
- Pilot Program: Develop and test the model in a controlled, non-live environment (a “silent pilot”) to assess its performance against historical data.
- Clinical Validation: Conduct a prospective study to validate the model’s performance in a real-world setting, comparing its outputs to the existing standard of care. This step is crucial for regulatory approval and clinician buy-in.
- Workflow Integration: The most critical step is seamlessly integrating the AI tool into the clinical workflow. If it adds clicks or disrupts established processes, adoption will fail. Strategies for 2025 and beyond must prioritize deep integration with primary systems like the EHR.
- Continuous Monitoring and Iteration: Deployed models must be continuously monitored for performance degradation or concept drift. A plan for periodic retraining and updating is essential.
Measuring success: Clinical outcomes, cost and adoption metrics
The success of Artificial Intelligence in Healthcare cannot be measured by algorithmic accuracy alone. A holistic evaluation framework is necessary to demonstrate true value.
| Metric Category | Key Performance Indicators (KPIs) |
|---|---|
| Clinical Outcomes | Improved diagnostic accuracy, reduced mortality rates, decreased length of stay, lower complication rates. |
| Operational Efficiency | Reduced patient wait times, increased throughput, optimized resource utilization, time saved per clinician. |
| Financial Impact | Cost savings from reduced waste, improved billing accuracy, lower readmission penalties, return on investment (ROI). |
| User Adoption and Satisfaction | Clinician adoption rates, user satisfaction scores, qualitative feedback on workflow integration. |
Barriers and common misconceptions
Navigating the implementation of AI requires addressing several common challenges and dispelling myths.
- The “Black Box” Problem: While some deep learning models are complex, the field of explainable AI (XAI) is advancing rapidly. The goal is not always full transparency but providing sufficient insight for a clinician to trust a recommendation.
- Fear of Job Replacement: The dominant narrative should be one of augmentation, not automation. AI is a tool to handle data-intensive tasks, freeing clinicians to focus on complex reasoning, patient communication, and empathy.
- Data Fragmentation: Healthcare data often resides in siloed systems. A major prerequisite for scalable AI is investment in data interoperability and building unified data platforms.
- Overestimation of “Plug-and-Play” Solutions: AI models are not universal. A model trained on data from one hospital population may not perform well in another. Local validation and calibration are essential.
Forward view: Autonomous systems and cognitive augmentation
Looking ahead, the role of Artificial Intelligence in Healthcare will continue to evolve from simple task assistance to more profound cognitive partnerships. Future systems will likely possess a greater degree of autonomy for well-defined, low-risk tasks, such as automated screening or protocol-driven dose adjustments. The ultimate vision is one of cognitive augmentation, where AI acts as a seamless extension of the clinician’s own expertise, synthesizing vast streams of real-time data to present insights and options that enhance, rather than replace, human judgment. This future requires a continued commitment to safety, ethics, and a human-centered design philosophy.
Appendix: Glossary, methodology and curated readings
Glossary of Key Terms
- AI (Artificial Intelligence): The theory and development of computer systems able to perform tasks that normally require human intelligence.
- DL (Deep Learning): A subset of machine learning using multi-layered neural networks to learn from vast amounts of data.
- EHR (Electronic Health Record): A digital version of a patient’s paper chart.
- NLP (Natural Language Processing): A field of AI focused on enabling computers to understand and process human language.
- ROI (Return on Investment): A performance measure used to evaluate the efficiency of an investment.
Methodology
The insights and recommendations in this whitepaper are based on a comprehensive review of peer-reviewed scientific literature, industry reports, and established best practices in clinical informatics and data science. The focus is on evidence-driven applications and practical implementation frameworks.