Table of Contents
- Introduction — Scope and clinical relevance
- How modern AI methods work: machine learning, deep learning and large language models
- Clinical application areas: diagnostics, workflow automation, patient monitoring, predictive analytics
- Data foundations: quality, labeling and interoperability
- Governance and responsible AI: bias mitigation, transparency and consent
- Regulatory and safety considerations for medical AI
- Implementation roadmap: pilot to scale
- Integration with clinical workflows and change management
- Common pitfalls and how to avoid them
- Future directions: research trends and emerging models
- Conclusion — Practical next steps for clinical teams
Introduction — Scope and clinical relevance
Artificial intelligence is no longer a concept confined to science fiction; it is rapidly becoming an indispensable tool within the clinical environment. For clinicians, hospital administrators, and health data scientists, understanding the practical application of Artificial Intelligence in Healthcare is crucial for navigating the future of medicine. This technology promises to enhance diagnostic accuracy, streamline administrative workflows, and enable personalized patient care on an unprecedented scale. The goal is not to replace human expertise but to augment it, empowering healthcare professionals with data-driven insights to improve patient outcomes.
This guide provides a practical roadmap for implementing AI in a clinical setting. We will move beyond the hype to explore the foundational technologies, real-world applications, ethical considerations, and step-by-step strategies for successful deployment. By focusing on a practical, evidence-based approach, this article aims to equip care teams with the knowledge needed to harness the transformative potential of Artificial Intelligence in Healthcare responsibly and effectively.
How modern AI methods work: machine learning, deep learning and large language models
At its core, modern Artificial Intelligence in Healthcare is driven by a set of powerful computational techniques. Understanding these methods is the first step toward appreciating their clinical potential and limitations.
-
Machine Learning (ML): This is a subset of AI where algorithms are trained on large datasets to recognize patterns and make predictions without being explicitly programmed for that specific task. For example, an ML model can be trained on patient data to predict the likelihood of hospital readmission based on factors like age, comorbidities, and length of stay.
-
Deep Learning (DL): A more advanced form of machine learning, deep learning uses complex, multi-layered “neural networks” inspired by the human brain’s structure. These networks excel at identifying intricate patterns in large, unstructured datasets. This makes DL particularly powerful for medical image analysis, such as detecting cancerous lesions in pathology slides or identifying subtle abnormalities on an MRI scan.
-
Large Language Models (LLMs): A recent breakthrough in deep learning, LLMs are trained on vast amounts of text data to understand, summarize, generate, and translate human language. In healthcare, their applications include summarizing lengthy patient records, drafting clinical notes, and powering conversational AI to help patients manage their care plans.
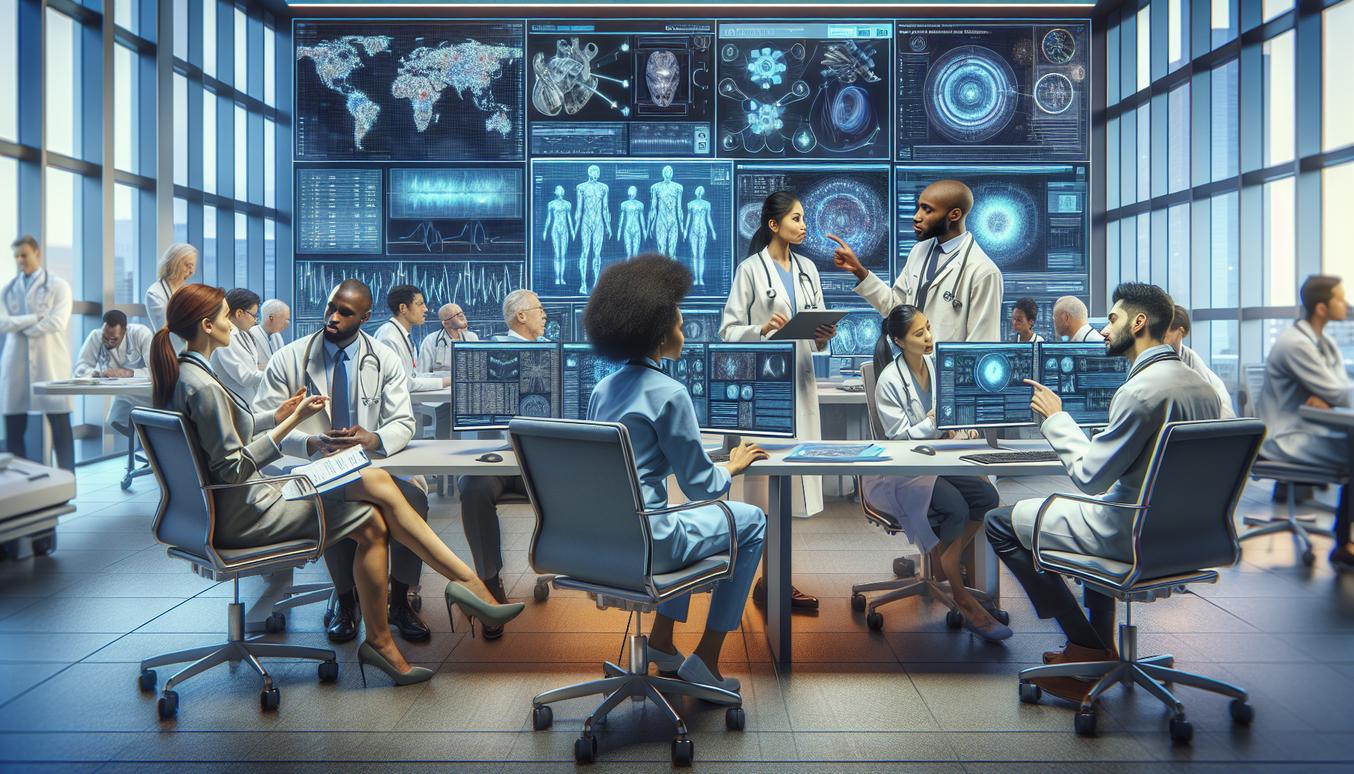
Clinical application areas: diagnostics, workflow automation, patient monitoring, predictive analytics
The applications of Artificial Intelligence in Healthcare span the entire patient journey, from initial diagnosis to ongoing management. These tools are designed to support clinical decision-making and optimize operational efficiency.
-
Diagnostics: AI algorithms are proving highly effective in interpreting medical imagery. They can analyze X-rays, CT scans, and retinal scans to flag potential issues for review by a specialist, often with a level of precision that matches or exceeds human capability. This accelerates the diagnostic process and can help catch diseases earlier.
-
Workflow Automation: A significant portion of a clinician’s time is spent on administrative tasks. AI can automate routine processes like scheduling appointments, managing medical billing, and transcribing voice notes into the electronic health record (EHR), freeing up valuable time for direct patient care.
-
Patient Monitoring: With the rise of wearable devices, AI can continuously analyze streams of data—such as heart rate, glucose levels, and activity patterns—to detect early signs of health deterioration. This is particularly valuable for managing chronic conditions like diabetes and heart failure, enabling proactive interventions.
-
Predictive Analytics: By analyzing historical patient data, predictive models can identify individuals at high risk for developing specific conditions, such as sepsis in hospitalized patients or a future cardiac event. This allows care teams to implement preventative measures and allocate resources more effectively.
Example vignette: AI assisted diagnostic pathway in radiology
Consider a 65-year-old patient who presents to the emergency department with a persistent cough. A chest CT scan is ordered to rule out serious pathology. The images are sent to the Picture Archiving and Communication System (PACS), where an AI algorithm immediately analyzes them. The AI flags a small, suspicious-looking pulmonary nodule and assigns it a high probability score for malignancy. This alert is instantly pushed to the on-call radiologist’s worklist, highlighted for urgent review. The radiologist examines the AI’s finding, confirms its presence, and measures it. Because the AI brought the potential issue to their attention immediately, the radiologist is able to issue a critical finding report within minutes instead of hours. This rapid, AI-assisted diagnosis allows the clinical team to schedule a biopsy and initiate a care plan much faster, significantly improving the patient’s prognosis. Here, the AI acts as a vigilant assistant, enhancing the radiologist’s workflow and diagnostic confidence.
Data foundations: quality, labeling and interoperability
The performance of any AI system is fundamentally dependent on the data it is trained on. The principle of “garbage in, garbage out” is especially true in healthcare. Establishing a robust data foundation is non-negotiable.
-
Data Quality: AI models require data that is accurate, complete, and representative of the patient population you intend to serve. Incomplete EHR entries, inconsistent terminology, and missing values can all degrade a model’s performance and lead to unreliable predictions.
-
Data Labeling: For many applications (especially in diagnostics), AI models need to be trained on expertly annotated data. This means clinicians, such as radiologists or pathologists, must label data—for example, by drawing boundaries around tumors on images. This process is time-consuming but essential for teaching the AI to recognize specific clinical features accurately.
-
Interoperability: Healthcare data often resides in separate, siloed systems (EHRs, lab systems, imaging archives). Interoperability is the ability for these different systems to exchange and interpret data seamlessly. Standards like Fast Healthcare Interoperability Resources (FHIR) are critical for creating the comprehensive datasets needed to train and deploy effective AI models across an organization.
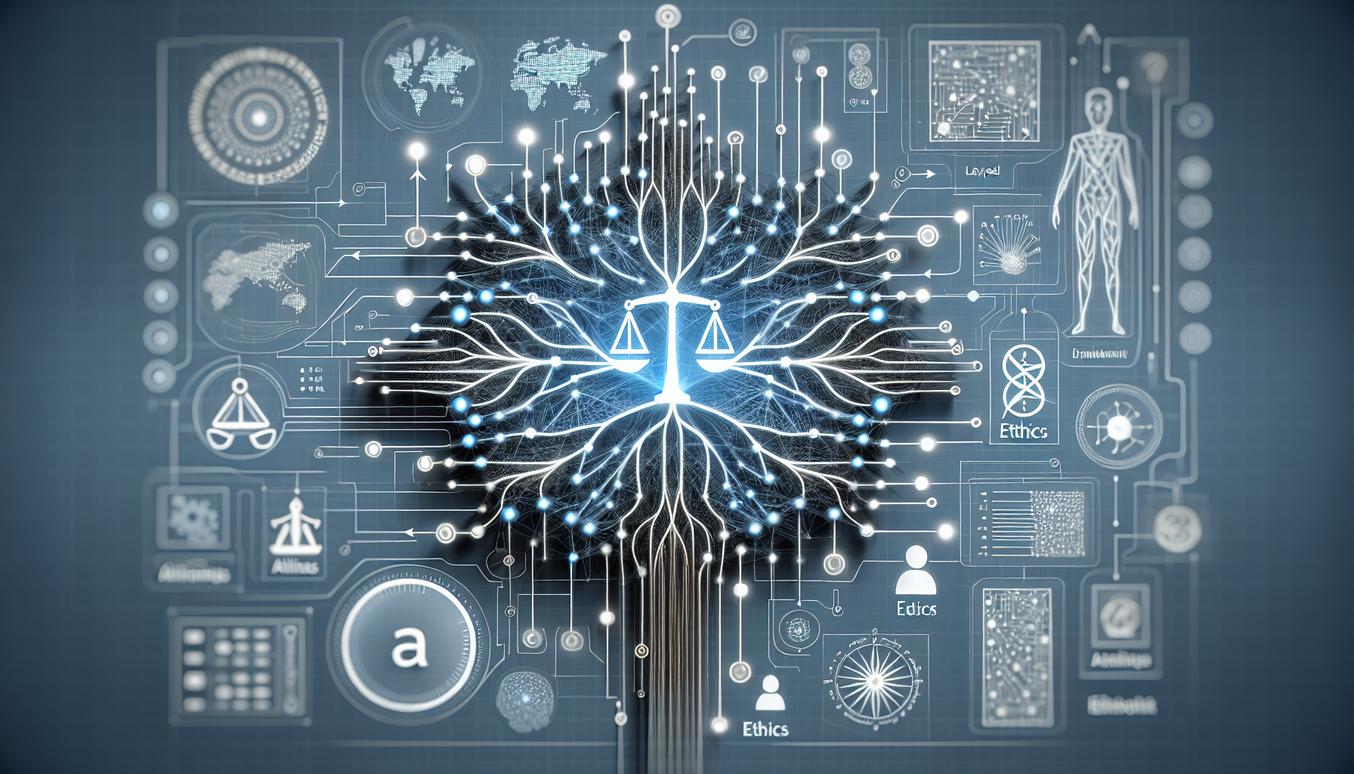
Governance and responsible AI: bias mitigation, transparency and consent
Deploying Artificial Intelligence in Healthcare carries significant ethical responsibilities. A strong governance framework is essential to ensure that AI is used safely, fairly, and transparently.
-
Bias Mitigation: AI models trained on historical data can inherit and even amplify existing biases related to race, gender, or socioeconomic status. For instance, an algorithm trained primarily on data from one demographic group may perform poorly for others. Bias mitigation involves auditing datasets for imbalances and testing model performance across different subpopulations to ensure equitable outcomes.
-
Transparency and Explainability: Clinicians are unlikely to trust a “black box” algorithm whose reasoning is opaque. Explainable AI (XAI) refers to methods that help humans understand why an AI model made a particular prediction. For example, an imaging AI might highlight the specific pixels in an X-ray that led to its conclusion, allowing a clinician to verify its logic.
-
Consent: The use of patient data for developing and deploying AI raises important privacy and consent issues. Healthcare organizations must have clear policies regarding how patient data is used, ensuring compliance with regulations like HIPAA. Patients should be informed about how their de-identified data contributes to improving care through AI.
Ethical checklist for clinical deployment
Before deploying an AI tool, clinical teams should review the following ethical considerations:
| Principle | Checklist Question |
|---|---|
| Fairness | Has the model been audited for performance disparities across different demographic groups (e.g., age, race, gender)? |
| Transparency | Can the model’s output be explained in a way that is clinically meaningful and understandable to the end-user? |
| Accountability | Is there a clear line of responsibility for clinical decisions made with AI assistance? Who is accountable if the AI makes an error? |
| Privacy | Are robust data security and de-identification measures in place to protect patient privacy at all stages? |
| Beneficence | Is there clear evidence that this AI tool will lead to improved patient outcomes or significant workflow efficiencies? |
| Non-maleficence | Has the model been rigorously validated to ensure it does not cause patient harm? Is there a plan for monitoring for unintended consequences? |
Regulatory and safety considerations for medical AI
AI tools used for clinical purposes are often classified as medical devices and are subject to regulatory oversight. In the United States, the United States Food and Drug Administration (FDA) plays a key role in ensuring the safety and effectiveness of medical AI. Understanding this landscape is crucial for hospital administrators and compliance officers.
A key concept is Software as a Medical Device (SaMD), which refers to software intended for medical purposes that is not part of a hardware medical device. Many AI algorithms, from diagnostic tools to treatment planning software, fall into this category. The FDA has developed a regulatory framework tailored to the iterative nature of AI, which allows for modifications and updates based on real-world performance data. However, this requires robust post-market surveillance, where organizations must continuously monitor the AI’s performance after deployment to detect any degradation or unexpected behavior and report adverse events.
Implementation roadmap: pilot to scale
Successfully integrating Artificial Intelligence in Healthcare requires a structured, phased approach rather than a “big bang” rollout. This roadmap outlines key stages for moving from a small-scale experiment to an enterprise-wide solution.
-
Identify the Right Problem: Begin by identifying a high-impact clinical or operational problem where AI can provide a clear solution. Involve frontline clinicians in this process to ensure the chosen problem is relevant and the proposed solution would be valuable in their daily workflow.
-
Launch a Pilot Program (2025 Strategy): Starting in 2025, initiate a controlled pilot project with a well-defined scope. Select a small group of users and a specific patient population. Establish clear success metrics before the pilot begins, covering clinical, operational, and financial outcomes.
-
Validate and Refine: Rigorously test the AI tool’s performance in your local environment and against your own patient data. Compare its results to the existing standard of care. Use feedback from the pilot to refine the model and the workflow integration.
-
Phased Rollout: Once the pilot has proven successful, begin a phased rollout. Expand the deployment to another department or a larger group of users. This allows your team to manage training and address any new challenges that arise with increased scale.
-
Scale and Monitor: After successful phased rollouts, move to full-scale implementation. This stage is not the end of the journey. Continuous monitoring of the AI’s performance and impact is essential for long-term success and safety.
Key performance indicators and monitoring post deployment
To measure the success of an AI implementation, it’s vital to track a balanced set of Key Performance Indicators (KPIs).
-
Clinical KPIs: These measure the impact on patient care. Examples include improvements in diagnostic accuracy, reduction in time-to-diagnosis or time-to-treatment, and adherence to clinical guidelines.
-
Operational KPIs: These focus on efficiency and workflow. Examples include reduction in clinician administrative time, improved patient throughput, and user satisfaction scores from clinicians.
-
Technical KPIs: These monitor the health of the AI system itself. Examples include model accuracy over time (to detect “model drift”), system uptime, and the speed of analysis.
Integration with clinical workflows and change management
Even the most accurate AI tool will fail if it is difficult to use or disrupts established clinical workflows. Seamless integration is paramount. The AI system should ideally operate within the software clinicians already use, such as the EHR or PACS, presenting its insights at the point of care without requiring users to log in to a separate application.
Equally important is change management. Introducing AI is not just a technical project; it is a cultural one. To ensure adoption and success, organizations must:
-
Involve Clinicians Early: Engage end-users in the selection, design, and validation process to build trust and ensure the tool meets their needs.
-
Provide Comprehensive Training: Educate staff not only on how to use the tool but also on its capabilities and limitations. Transparency about how the AI works helps build confidence.
-
Establish Feedback Loops: Create a clear channel for users to report issues, provide suggestions, and ask questions. This fosters a sense of ownership and allows for continuous improvement.
Common pitfalls and how to avoid them
Many organizations encounter similar challenges when implementing Artificial Intelligence in Healthcare. Awareness of these common pitfalls can help you navigate around them.
-
Pitfall: Solving a non-existent problem.
Avoidance: Start with a clear clinical need identified by frontline staff, not with a technology looking for a problem. -
Pitfall: Underestimating data preparation.
Avoidance: Allocate significant time and resources for data cleaning, integration, and governance before beginning model development. -
Pitfall: Neglecting workflow integration.
Avoidance: Map out the existing clinical workflow and design the AI integration to be as seamless and intuitive as possible from the very beginning. -
Pitfall: Lack of robust clinical validation.
Avoidance: Do not rely solely on the vendor’s performance claims. Conduct an independent, prospective validation of the AI tool with your own patient population before a wide rollout. -
Pitfall: Forgetting the human element.
Avoidance: Develop a comprehensive change management and training plan. Communicate openly and address the concerns of clinical staff to build trust and encourage adoption.
Future directions: research trends and emerging models
The field of Artificial Intelligence in Healthcare is evolving at a breathtaking pace, with several exciting research trends poised to shape the next generation of clinical tools. Global health organizations like the World Health Organization and research bodies like the National Institutes of Health are actively exploring these frontiers. For the latest research, clinicians and scientists can follow leading journals such as Nature Medicine and the Journal of the American Medical Association.
-
Federated Learning: This approach allows AI models to be trained across multiple hospitals or research centers without the sensitive patient data ever leaving its source institution. This enhances data privacy while enabling the creation of more robust and generalizable models.
-
Multimodal AI: Future AI systems will increasingly integrate and analyze different types of data simultaneously. A multimodal model could combine a patient’s medical images, genomic data, lab results, and clinical notes to generate a far more holistic and accurate diagnostic or prognostic assessment.
-
Generative AI and Drug Discovery: Beyond summarizing text, generative AI models are being used to design novel proteins and molecules, dramatically accelerating the drug discovery and development process by predicting which compounds are most likely to be effective against a specific disease.
Conclusion — Practical next steps for clinical teams
Artificial Intelligence in Healthcare is a powerful force for positive transformation, offering the potential to enhance clinical decision-making, improve efficiency, and personalize patient care. However, its successful implementation is not merely a technical challenge; it is a strategic one that requires careful planning, clinical leadership, and a steadfast commitment to ethical principles.
For clinical teams looking to begin their AI journey, the path forward is one of deliberate, incremental steps. Here are four practical next actions:
-
Form a Multidisciplinary Steering Committee: Assemble a team that includes clinicians, IT specialists, data scientists, and hospital administrators. This group will provide the balanced perspective needed to guide your organization’s AI strategy.
-
Identify a Single, High-Impact Pilot Project: Do not try to boil the ocean. Select one well-defined problem where AI can deliver clear, measurable value. Success in a small-scale pilot will build momentum for future initiatives.
-
Assess Your Data Readiness: Begin a thorough assessment of your organization’s data quality, governance, and interoperability. A strong data foundation is the prerequisite for any successful AI endeavor.
-
Educate and Engage Your Teams: Foster a culture of responsible innovation by educating staff about both the potential and the limitations of AI. Engage them in the process to build the trust and buy-in necessary for lasting change.
By embracing a thoughtful, human-centered approach, healthcare organizations can unlock the immense promise of AI to build a more efficient, effective, and equitable future for medicine.