A Leader’s Guide to Implementing Artificial Intelligence in Healthcare: The 2025 Playbook
Table of Contents
- Executive Summary
- Why AI Matters in Modern Care
- Core Concepts Clinicians Should Know
- Clinical Applications and Concise Case Studies
- Data Collection, Labeling and Governance
- Choosing Models and Validation Strategies
- Deployment Roadmap for Hospitals and Clinics
- Integration with Clinical Workflows and EHR Systems
- Regulatory, Ethics and Governance Checklist
- Measuring Outcomes and Continuous Monitoring
- Risk Mitigation and Common Pitfalls
- Research Gaps and Future Directions
- Appendix: Tools, Metrics and Reading List
Executive Summary
This guide serves as a practical playbook for healthcare leaders and data scientists navigating the implementation of Artificial Intelligence in Healthcare. It moves beyond theoretical discussions to provide a structured approach for integrating AI into clinical practice. We cover foundational concepts, present actionable case studies, and outline a step-by-step roadmap for deployment. Key takeaways include the critical importance of high-quality data governance, robust model validation, and a steadfast commitment to ethical principles. By pairing clinical applications with reproducible validation steps and a comprehensive governance checklist, this document aims to empower organizations to harness the transformative potential of AI to improve patient outcomes and operational efficiency.
Why AI Matters in Modern Care
The landscape of modern medicine is undergoing a profound transformation, shifting from a reactive model to one that is proactive, predictive, and personalized. Artificial Intelligence in Healthcare is the engine driving this change. Healthcare systems generate a staggering volume of data daily, from electronic health records (EHRs) and medical imaging to genomic sequences and wearable device metrics. Human cognitive capacity alone is insufficient to synthesize this information effectively. AI provides the tools to analyze these complex datasets at scale, uncovering patterns and insights that can lead to earlier diagnoses, more effective treatments, and streamlined hospital operations. This technology is not about replacing clinicians but augmenting their expertise, freeing them from repetitive tasks to focus on complex patient care and decision-making.
Core Concepts Clinicians Should Know
A foundational understanding of AI terminology is essential for effective collaboration between clinical and technical teams. Here are the core concepts that healthcare professionals should be familiar with.
Machine Learning and Deep Learning
At its core, Machine learning (ML) is a subset of AI where algorithms are trained on data to make predictions or decisions without being explicitly programmed for the task. Deep Learning is a more advanced subfield of ML that uses complex, multi-layered Neural Networks to learn from vast amounts of data. This is the technology behind many of the most significant breakthroughs in medical imaging analysis.
Supervised vs. Unsupervised Learning
Understanding the two primary types of learning is crucial for identifying the right approach for a clinical problem.
- Supervised Learning: The algorithm learns from a dataset that has been manually labeled with the correct outcomes. For example, training a model on thousands of retinal scans labeled by ophthalmologists as having “diabetic retinopathy” or “no diabetic retinopathy.”
- Unsupervised Learning: The algorithm works with unlabeled data to identify hidden patterns or structures. A common application is patient stratification, where it can group patients with similar characteristics into distinct cohorts that may respond differently to treatment.
Natural Language Processing (NLP)
Natural Language Processing (NLP) is a branch of AI that gives computers the ability to understand, interpret, and generate human language. In healthcare, NLP is used to extract structured information from unstructured text, such as clinician’s notes, pathology reports, and scientific literature, making this valuable data accessible for analysis and clinical decision support.
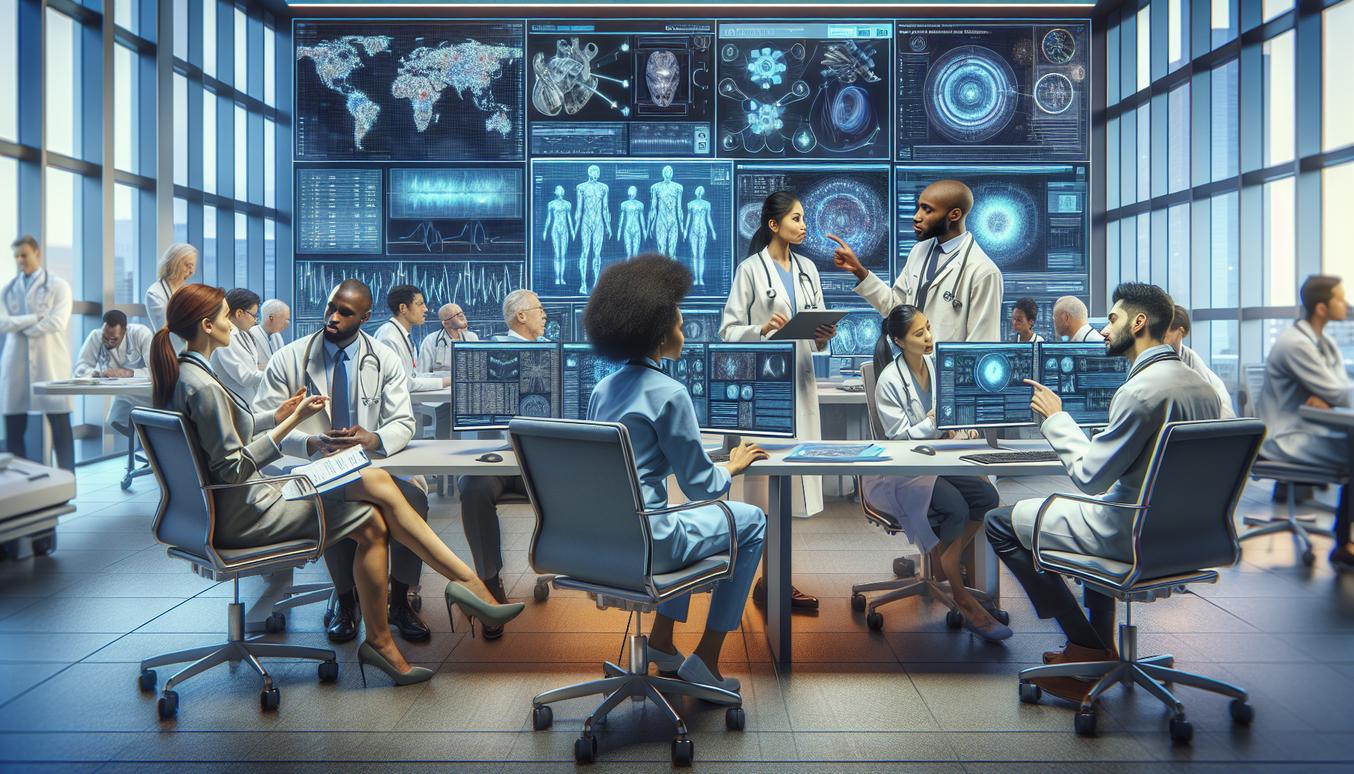
Clinical Applications and Concise Case Studies
The application of Artificial Intelligence in Healthcare spans numerous specialties. Here are three concise case studies illustrating its impact.
Case Study 1: Medical Imaging Analysis
A deep learning model, specifically a Convolutional Neural Network (CNN), is trained on a large, curated dataset of chest X-rays. The model learns to identify the subtle patterns associated with pneumonia. When deployed, it acts as a triage tool, flagging suspected positive cases for priority review by a radiologist. Validation Step: The model’s performance is validated against a hold-out test set of images annotated by a consensus panel of three radiologists, measuring its sensitivity and specificity to ensure it meets clinical standards before deployment.
Case Study 2: Predictive Analytics for Sepsis Onset
An ML model is developed using real-time data from a hospital’s EHR, including vital signs, lab results, and medication history. The model continuously calculates a patient’s risk score for developing sepsis in the intensive care unit (ICU). When the risk score exceeds a certain threshold, it triggers an alert in the EHR for the clinical team to review. Validation Step: The model is validated retrospectively on historical patient data from the past year and then prospectively in a silent, non-interventional mode to measure its predictive accuracy and false alert rate in a real-world setting.
Case Study 3: Personalized Oncology Treatment
An AI platform analyzes a patient’s genomic data from a tumor biopsy, alongside their clinical history and relevant medical literature. It identifies specific mutations and recommends targeted therapies that have shown efficacy for similar genomic profiles. This supports the oncologist in making a more informed, personalized treatment decision. Validation Step: The AI’s recommendations are compared against the decisions made by a molecular tumor board for a cohort of patients. The concordance rate and any novel, evidence-backed suggestions from the AI are documented.
Data Collection, Labeling and Governance
A successful AI initiative is built on a foundation of high-quality, well-governed data. Garbage in, garbage out is the immutable law of machine learning.
Sourcing High-Quality Data
The most effective models are trained on large, diverse, and representative datasets. Key sources include Picture Archiving and Communication Systems (PACS) for imaging, EHRs for clinical data, and specialized genomic or pathology databases. It is crucial to ensure the data reflects the patient population the model will be used on to avoid inherent bias.
The Critical Role of Labeling
For supervised learning, the accuracy of data labels is paramount. This process often requires significant time from clinical experts, such as radiologists annotating tumors on a CT scan or pathologists labeling cell types. Investing in robust labeling tools and clear annotation guidelines is a non-negotiable step for building a reliable clinical AI model.
Data Governance Framework
A strong governance framework is essential. This includes establishing clear policies for:
- Data Privacy and Security: Ensuring full compliance with regulations like HIPAA in the U.S. or GDPR in Europe. All patient data must be de-identified or anonymized whenever possible.
- Data Access: Defining who can access data and for what purpose, with clear audit trails.
- Data Quality: Implementing automated checks and manual reviews to ensure data is accurate, complete, and consistent.
Choosing Models and Validation Strategies
Selecting the right model and rigorously validating its performance are critical technical steps.
Model Selection Considerations
The choice of model involves a trade-off. Simpler models like logistic regression are highly interpretable but may lack the predictive power for complex tasks. In contrast, deep learning models can achieve state-of-the-art performance but are often considered “black boxes,” making their reasoning difficult to understand. The choice depends on the clinical use case; for high-stakes decisions, explainability may be as important as accuracy.
Robust Validation Techniques
Never validate a model on the same data it was trained on. Best practices include:
- Cross-Validation: The training data is split into multiple subsets, and the model is trained and validated multiple times to ensure its performance is stable and not dependent on a specific data split.
- Hold-out Test Set: A completely separate dataset, unseen by the model during training, is used for the final evaluation. This provides the most realistic estimate of how the model will perform on new patients.
- External Validation: The ultimate test is to validate the model’s performance on data from a different hospital or patient population to assess its generalizability.
Deployment Roadmap for Hospitals and Clinics
A phased approach to deployment minimizes risk and helps build institutional trust. A realistic timeline for integrating Artificial Intelligence in Healthcare begins in 2025.
Phase 1 (2025): Pilot and Proof-of-Concept
Start with a well-defined clinical problem with a high potential for impact and measurable outcomes. Form a multidisciplinary team including clinicians, data scientists, IT staff, and hospital administrators. The goal is to develop a proof-of-concept model and demonstrate its potential value in a controlled, offline environment.
Phase 2 (2026): Limited Clinical Rollout
After successful validation, deploy the AI tool in a limited, controlled clinical setting. For example, an imaging AI could run in the background as a “second reader” or a predictive model could generate alerts that are reviewed by a specialized team before reaching the primary clinician. This phase is crucial for gathering user feedback and identifying workflow integration challenges.
Phase 3 (2027 and Beyond): Scaled Deployment and Expansion
Based on the outcomes and learnings from the limited rollout, the AI tool can be fully integrated into the clinical workflow. This involves deep integration with the EHR, training for all relevant staff, and establishing a continuous monitoring process. Success in one area can then serve as a blueprint for expanding AI initiatives to other departments.
Integration with Clinical Workflows and EHR Systems
An AI model is only valuable if its insights are delivered to the clinician at the right time and in the right context. This requires seamless technical and workflow integration. A primary challenge is interoperability between the AI application and the existing EHR system. Adopting modern data exchange standards like FHIR (Fast Healthcare Interoperability Resources) is critical for enabling this communication. Furthermore, the user interface must be designed with clinician input to ensure that AI-generated insights are presented clearly and intuitively, supporting, rather than disrupting, the decision-making process.
Regulatory, Ethics and Governance Checklist
Implementing Artificial Intelligence in Healthcare carries significant ethical responsibilities. As highlighted by organizations like the World Health Organization, a strong ethical framework is not optional. Use this checklist as a starting point for governance.
- Regulatory Compliance: Have you determined if your AI tool qualifies as a Software as a Medical Device (SaMD)? Are you following all relevant guidelines from regulatory bodies like the FDA?
- Algorithmic Fairness and Bias: Has the model been audited for performance disparities across different demographic groups (e.g., race, gender, socioeconomic status)? Was the training data representative of your target patient population?
- Transparency and Explainability: For high-stakes decisions, can the model’s output be explained? Can a clinician understand why the AI made a particular recommendation?
- Patient Privacy and Consent: Do you have clear policies for data de-identification? Is there a process for informing patients about how their data is used for AI model development and deployment?
- Accountability and Responsibility: Is there a clear protocol for what happens when an AI model makes an error? Who is accountable—the developer, the hospital, or the clinician?
Measuring Outcomes and Continuous Monitoring
The success of an AI implementation must be measured by its real-world impact. Beyond technical metrics like accuracy, organizations should track:
- Clinical Outcomes: Did the AI tool contribute to improved patient outcomes, such as reduced length of stay, lower readmission rates, or earlier cancer detection?
- Operational Efficiency: Did the tool improve workflows, reduce costs, or save clinician time? For example, did it shorten the time required to read a medical scan?
- Clinician and Patient Satisfaction: Are the users of the tool—both clinicians and patients—satisfied with its performance and usability?
Furthermore, models require continuous monitoring for performance degradation, a phenomenon known as “model drift.” This can happen as patient populations, clinical practices, or medical equipment change over time. A plan for periodic retraining and re-validation is essential.
Risk Mitigation and Common Pitfalls
Proactive risk mitigation can prevent common AI projects from failing. The table below outlines frequent pitfalls and corresponding strategies.
| Common Pitfall | Mitigation Strategy |
|---|---|
| Poor Data Quality or “Data Silos” | Invest in a robust data governance framework and data engineering resources before starting model development. |
| Overfitting the Model | Use rigorous validation techniques like cross-validation and a hold-out test set to ensure the model generalizes to new data. |
| Lack of Clinician Buy-In | Engage clinical stakeholders from day one. Frame the project around solving their problems and involve them in the design and validation process. |
| The “Black Box” Problem | For critical decisions, prioritize models with high interpretability or use Explainable AI (XAI) techniques to provide insight into model predictions. |
| EHR Integration Failures | Plan for technical integration from the project’s inception. Utilize modern interoperability standards like FHIR and conduct thorough testing. |
Research Gaps and Future Directions
The field of Artificial Intelligence in Healthcare is evolving rapidly. As noted in comprehensive reviews by institutions like the NIH, several key areas are poised for significant advancement:
- Federated Learning: This approach allows models to be trained across multiple hospitals without centralizing sensitive patient data, thus enhancing privacy and data access.
- Causal AI: Moving beyond correlation to understand causation. This will enable AI to not just predict an outcome but to suggest interventions that can change it.
- Generative AI: Using models to generate high-quality synthetic data to augment small datasets or to assist in automating clinical documentation and reporting.
Appendix: Tools, Metrics and Reading List
Common Tools
- Programming Languages: Python is the standard, with essential libraries like TensorFlow, PyTorch, and Scikit-learn for building and training models.
- Platforms: Major cloud providers (AWS, Google Cloud, Azure) offer HIPAA-compliant services and specialized AI/ML platforms tailored for healthcare workloads.
Key Performance Metrics
- Accuracy: The proportion of total predictions that were correct. Can be misleading in datasets with class imbalance.
- Precision: Of all the positive predictions, how many were actually correct? Important for minimizing false positives.
- Recall (Sensitivity): Of all the actual positive cases, how many did the model correctly identify? Crucial for minimizing false negatives in diagnostic tasks.
- AUC-ROC: A measure of the model’s ability to distinguish between classes. A value of 1.0 represents a perfect model.
Suggested Reading
- Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again by Eric Topol.
- WHO guidance on the ethics and governance of artificial intelligence for health.
- Regularly updated reviews and publications from major medical and scientific journals.