Table of Contents
- Introduction – Reframing Healthcare Challenges for AI Adoption
- AI Fundamentals for Clinical Use
- Key Clinical Applications and Use Cases
- Integrating AI into Clinical Workflows
- Data Quality, Privacy and Interoperability
- Validation, Safety and Governance
- Measuring Impact and Operational KPIs
- Case Studies – Practical Deployments and Lessons Learned
- Deployment Roadmap and Checklist
- Ethical Considerations and Responsible AI
- Appendix and Further Reading
Introduction – Reframing Healthcare Challenges for AI Adoption
The healthcare landscape is navigating unprecedented pressures: escalating operational costs, an increasing burden of chronic disease, and persistent challenges with clinician burnout. While technology has long been part of the clinical environment, the strategic implementation of Artificial Intelligence in Healthcare is moving from a futuristic concept to a present-day imperative. The conversation is no longer about whether AI will change healthcare, but how to deploy it responsibly, effectively, and sustainably.
This whitepaper moves beyond high-level theory to provide a practical, implementation-first guide for healthcare leaders. Our focus is on integrating AI as a tool to augment clinical intelligence, streamline operations, and ultimately improve patient outcomes. We will address the foundational technologies, critical use cases, and the essential frameworks for governance, validation, and workflow integration necessary for successful adoption. The goal is not to replace human expertise but to empower it with data-driven insights at scale, reframing persistent challenges as opportunities for innovation.
AI Fundamentals for Clinical Use
Understanding the core technologies behind Artificial Intelligence in Healthcare is the first step toward effective implementation. AI is a broad field, but for clinical applications, a few key sub-disciplines are paramount.
Machine Learning and Deep Learning in Practice
Machine Learning (ML) is a subset of AI where algorithms are trained on data to find patterns and make predictions without being explicitly programmed for that task. In the clinical context, this typically involves:
- Supervised Learning: The most common approach, where the algorithm learns from a dataset that is already labeled with known outcomes. For example, training a model on thousands of chest X-rays labeled by radiologists as “pneumonia” or “no pneumonia” to learn to identify the condition in new, unlabeled images.
- Unsupervised Learning: This method is used when data is not labeled. The algorithm sifts through the data to identify hidden patterns or structures on its own. This is useful for patient stratification, such as identifying distinct subgroups of diabetic patients based on their electronic health records (EHR) data who may respond differently to treatments.
Deep Learning is a more advanced form of machine learning that uses complex, multi-layered “neural networks” to analyze data. It has proven especially powerful in interpreting perceptual data like medical images. For instance, deep learning models can detect subtle patterns in retinal scans indicative of diabetic retinopathy, often with a level of accuracy comparable to or exceeding human specialists.
Natural Language Processing for Clinical Text
A vast amount of critical patient information is locked away in unstructured text, such as clinician notes, pathology reports, and discharge summaries. Natural Language Processing (NLP) is the branch of AI that gives computers the ability to understand, interpret, and generate human language. In healthcare, NLP enables:
- Information Extraction: Pulling structured data from unstructured notes, such as identifying patient medications, symptoms, and family history from a physician’s narrative.
- Clinical Documentation Improvement: Analyzing notes in real-time to prompt clinicians for greater specificity, which can improve billing accuracy and quality reporting.
- Data De-identification: Automatically removing protected health information (PHI) from clinical text to create datasets for research while maintaining patient privacy.
Key Clinical Applications and Use Cases
The application of Artificial Intelligence in Healthcare spans the entire patient journey, from diagnosis to treatment and operational management. The most mature and impactful use cases focus on augmenting human capabilities in data-intensive tasks.
Diagnostic Augmentation and Imaging Analytics
Medical imaging is a primary area where AI is delivering significant value. Algorithms trained on vast libraries of images can identify patterns that may be difficult for the human eye to detect, especially under time pressure. Key applications include:
- Radiology: Assisting in the detection of nodules on CT scans, identifying strokes in brain MRIs, and flagging suspicious lesions in mammograms for radiologist review. This serves as a “second read,” improving accuracy and reducing turnaround times.
- Pathology: Analyzing digital pathology slides to quantify tumor cells, identify mitotic figures, or screen for cancer, allowing pathologists to focus their attention on the most complex cases.
- Ophthalmology: Screening for conditions like diabetic retinopathy and age-related macular degeneration from retinal fundus images, enabling earlier detection in primary care settings.
Predictive Modelling for Patient Deterioration
One of the most promising areas for AI is in predicting adverse events before they happen, enabling proactive rather than reactive care. These models continuously analyze streams of data from the EHR to calculate risk scores.
- Sepsis Prediction: Identifying patients at high risk of developing sepsis by analyzing vital signs, lab results, and clinical notes, often hours earlier than traditional methods. This allows for timely intervention, which is critical for improving survival rates.
- Acute Kidney Injury (AKI): Forecasting the likelihood of a patient developing AKI, giving clinical teams a window to adjust medications or fluid management.
- Hospital Readmissions: Predicting which patients are at high risk for readmission upon discharge, allowing care teams to allocate transitional care resources more effectively.
Integrating AI into Clinical Workflows
An AI model with high predictive accuracy is clinically useless if it cannot be seamlessly integrated into existing workflows. Successful implementation hinges on human-centered design and robust technical architecture.
Human in the Loop and Decision Support Design
The most effective AI systems function as clinical co-pilots, not autopilots. The “human-in-the-loop” model ensures that a qualified clinician is always the final decision-maker. This requires careful design of the user interface and the information presented.
- Actionable Insights, Not Just Alerts: Instead of simply flashing a high-risk score, the system should present the key factors that contributed to the prediction (explainability). For a sepsis alert, this might include showing the specific vital sign trends and lab results that triggered it.
- Minimizing Alert Fatigue: Systems must be tuned to achieve a high signal-to-noise ratio. Too many false-positive alerts will cause clinicians to ignore the system entirely. This involves setting appropriate risk thresholds and allowing for customization based on unit-specific patient populations.
- Passive vs. Active Notifications: The urgency of the AI insight should determine how it is delivered. A prediction of long-term risk might be a passive note in the EHR, while an imminent risk of patient deterioration should trigger a direct, active alert to the appropriate care team member.
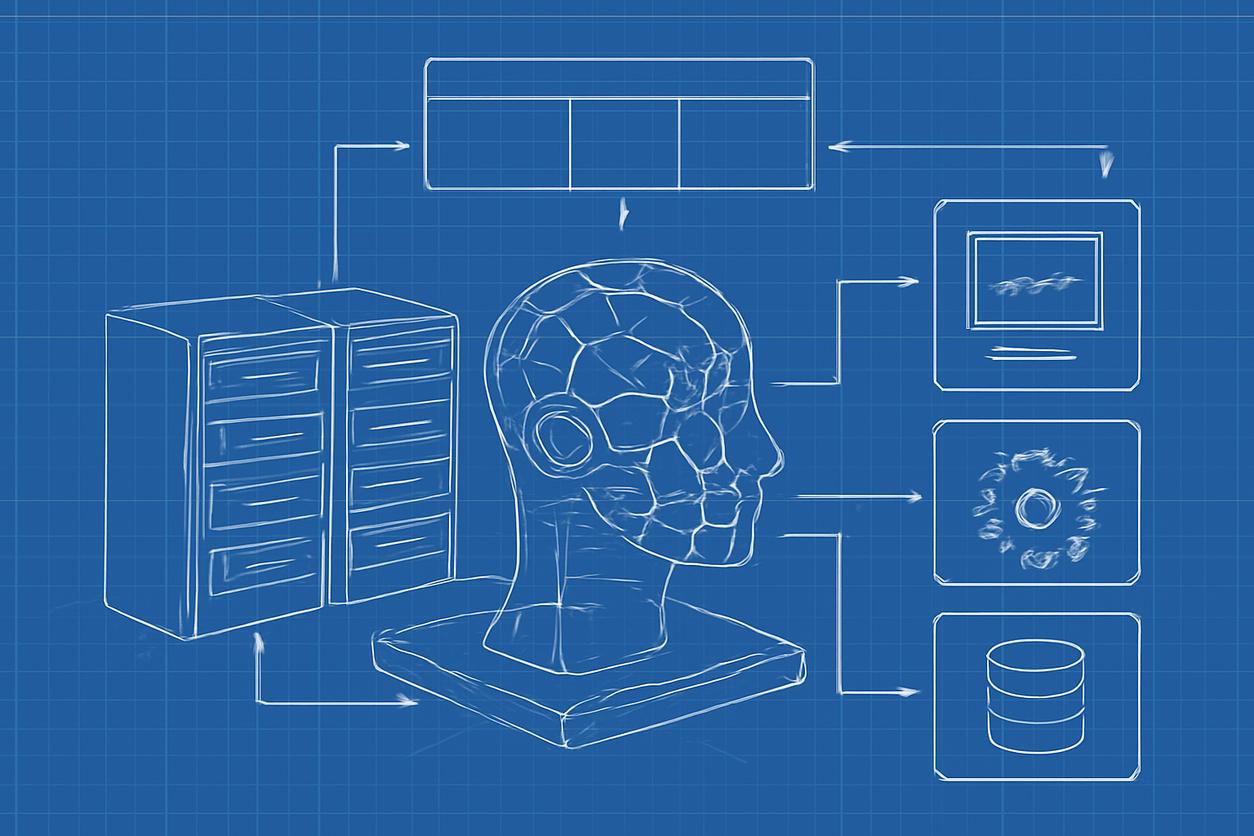
Interoperability and System Architecture Considerations
AI models need data, and that data often resides in siloed systems. A modern, interoperable architecture is non-negotiable for deploying Artificial Intelligence in Healthcare at scale.
- EHR Integration: The Electronic Health Record is the central hub of clinical workflow. AI tools must integrate directly with the EHR, both to pull real-time data for analysis and to push insights and recommendations back to the clinician at the point of care.
- Standardized Data Formats: Adherence to standards like FHIR (Fast Healthcare Interoperability Resources) is crucial. FHIR provides a common language for healthcare applications to exchange clinical and administrative data, simplifying the process of connecting an AI model to various data sources.
- Cloud vs. On-Premise: The decision to host AI infrastructure on-premise or in the cloud involves trade-offs in security, scalability, and cost. Hybrid models are often a practical solution, keeping sensitive patient data on-premise while leveraging the cloud’s computational power for model training.
Data Quality, Privacy and Interoperability
Data is the lifeblood of any AI system. The success of any initiative in Artificial Intelligence in Healthcare is directly dependent on the quality, accessibility, and security of the underlying data. A robust data strategy must precede any algorithm development.
Data Quality is paramount; the principle of “garbage in, garbage out” has never been more relevant. This involves ensuring data is accurate, complete, consistent, and timely. A data governance program is essential to establish and enforce standards for data entry and maintenance. Furthermore, data must be representative of the patient population it will be used on to avoid building biased models.
Protecting Patient Privacy is a legal and ethical obligation. All AI projects must be designed with privacy at their core, adhering strictly to regulations such as the Health Insurance Portability and Accountability Act (HIPAA). This includes implementing strong access controls, data encryption, and de-identification techniques when data is used for model training and research.
Validation, Safety and Governance
Trust is the currency of healthcare. For clinicians to adopt AI tools, they must be confident in their safety, accuracy, and reliability. This requires a rigorous framework for validation and governance.
Clinical Validation must go beyond retrospective testing on a static dataset. True validation involves prospective studies in the real-world clinical environment to measure the model’s performance and its actual impact on decision-making and patient outcomes. Regulatory bodies, such as the U.S. Food and Drug Administration, have specific pathways for “Software as a Medical Device” (SaMD) that outline requirements for safety and efficacy.
An institutional AI Governance Committee is a critical component of a responsible AI program. This multidisciplinary team—comprising clinicians, data scientists, IT specialists, ethicists, and administrators—should be responsible for:
- Reviewing and approving proposed AI projects.
- Setting standards for data quality and model validation.
- Monitoring the performance and safety of deployed models over time.
- Establishing policies for ethical use, bias mitigation, and transparency.
Measuring Impact and Operational KPIs
To justify investment and drive adoption, the value of Artificial Intelligence in Healthcare must be quantified. While technical metrics like model accuracy are important for development, the true measure of success lies in clinical and operational key performance indicators (KPIs).
Organizations should define target KPIs before deployment and continuously track them afterward. These metrics should align with the “Triple Aim” of healthcare: improving the patient experience, improving the health of populations, and reducing the per capita cost of care. A sample KPI table is shown below.
| Domain | Example KPI | AI Use Case Example |
|---|---|---|
| Clinical Outcomes | Sepsis-related mortality rate | Sepsis Prediction Model |
| Patient Safety | Adverse drug event rate | Medication Error Prediction |
| Operational Efficiency | Average patient length of stay | Discharge Planning Optimization |
| Clinician Experience | Time spent on clinical documentation | Ambient Clinical Voice Scribe |
| Access to Care | Wait time for radiology report | Imaging Triage and Prioritization |
Case Studies – Practical Deployments and Lessons Learned
Case Study 1: Sepsis Prediction in the ICU
An academic medical center deployed an AI-powered sepsis detection tool integrated with its EHR. The model continuously monitored patient data and alerted a dedicated rapid response nursing team when a patient’s risk score crossed a validated threshold. The alert included the specific factors driving the risk. Lessons Learned: The success was not just the algorithm but the creation of a new clinical workflow around the alert. A dedicated human response team was critical to filter alerts and ensure timely action, preventing alert fatigue among bedside clinicians.
Case Study 2: Optimizing Operating Room Scheduling
A large hospital system used a machine learning model to predict the duration of surgical procedures more accurately than traditional methods. The model analyzed historical data, including the surgeon, procedure type, and patient characteristics. The predictions were integrated into the scheduling system. Lessons Learned: Gaining surgeon trust was the biggest challenge. The project team achieved this by first running the model in a “silent” mode for several months, demonstrating its superior accuracy with real data before it was used to actively influence the schedule.
Deployment Roadmap and Checklist
A structured approach is essential for any organization embarking on an Artificial Intelligence in Healthcare journey. The following roadmap outlines key phases for a strategic rollout starting in 2025.
- Phase 1: Foundation and Strategy (2025)
- Establish an AI governance committee with multidisciplinary representation.
- Identify 2-3 high-impact clinical or operational problems to solve. Prioritize based on clinical need, data availability, and potential ROI.
- Conduct a data maturity assessment. Identify gaps in data quality, accessibility, and infrastructure.
- Develop a multi-year budget and resource plan.
- Phase 2: Pilot and Validation (2026)
- Select a vendor or develop an initial pilot model for the top-priority use case.
- Perform rigorous retrospective validation on internal data.
- Design the clinical workflow integration and define KPIs for success.
- Conduct a limited-scope, prospective pilot in a controlled environment (e.g., a single hospital unit).
- Phase 3: Scale and Monitor (2027 and Beyond)
- Based on pilot success, begin a phased rollout across the organization.
- Implement a continuous monitoring program to track model performance, clinical outcomes, and KPIs.
- Establish a feedback loop for clinicians to report issues and suggest improvements.
- Use learnings to inform the selection and development of the next set of AI initiatives.
Ethical Considerations and Responsible AI
The power of Artificial Intelligence in Healthcare comes with profound ethical responsibilities. A commitment to responsible AI is not optional; it is a prerequisite for building trust and ensuring equitable outcomes.
- Algorithmic Bias: AI models learn from historical data. If that data reflects existing health disparities, the model can perpetuate or even amplify them. It is crucial to audit datasets for potential biases (e.g., based on race, gender, or socioeconomic status) and use mitigation techniques during model development.
- Transparency and Explainability: While some complex “black box” models are highly accurate, clinicians need to understand why a model is making a particular recommendation. The field of Explainable AI (XAI) aims to develop techniques that can provide this transparency, which is vital for trust and accountability.
- Accountability: When an AI system contributes to a clinical error, who is responsible? The clinician, the hospital, or the AI developer? Clear policies must be established for accountability, outlining the roles and responsibilities of all stakeholders in the development, deployment, and use of clinical AI.
- Patient Consent: Health systems must be transparent with patients about how their data is being used to develop and power AI systems. Clear communication and consent processes are fundamental to maintaining patient trust.
Appendix and Further Reading
For leaders seeking to deepen their understanding of Artificial Intelligence in Healthcare, the following resources provide valuable information on global health policy, research, and regulation.
- World Health Organization: Offers guidance and reports on the ethics and governance of artificial intelligence for health on a global scale.
- National Institutes of Health: Funds and conducts extensive research into the development and application of AI and machine learning in biomedical science.
- PubMed: A comprehensive database of biomedical literature, containing countless peer-reviewed studies on the validation and impact of AI in various clinical specialties.
- U.S. Food and Drug Administration: Provides the regulatory framework for AI/ML-based software as a medical device, including guidelines on approval and post-market surveillance.