Table of Contents
- Introduction and Scope
- Foundational Methods: Neural Networks, Deep Learning and Reinforcement Learning
- Natural Language Processing for Clinical Text
- Imaging and Signal Analysis: Beyond Radiology
- Predictive Modeling for Patient Risk and Personalized Care
- Operational Automation: Clinical Workflow and Administrative Tasks
- Data Quality, Standards and Interoperability
- Validation, Performance Metrics and Real-World Evaluation
- Ethical Safeguards and Responsible AI Governance
- Privacy, Security and Data Stewardship
- Implementation Roadmap: Pilot to Scale with Checklist
- Common Pitfalls and Mitigation Strategies
- Emerging Trends: Autonomous Systems and Cognitive Computing
- Curated Resources and Further Reading
- Summary and Practical Next Steps
Introduction and Scope
The integration of Artificial Intelligence in Healthcare represents a paradigm shift, moving from reactive treatment to proactive, predictive, and personalized medicine. This technology is no longer a futuristic concept but a rapidly evolving set of tools being actively deployed to augment clinical decision-making, streamline operations, and accelerate biomedical research. For clinicians, researchers, and health IT leaders, understanding the practical applications, implementation challenges, and ethical guardrails of AI is now a critical competency.
This guide provides an authoritative yet approachable overview of Artificial Intelligence in Healthcare. We will move beyond the hype to offer a practical framework for its evaluation and adoption. The focus is on real-world clinical integration, covering foundational methods, key application areas, and the essential pillars of data governance, validation, and ethics. Our goal is to equip you with the knowledge to navigate this complex landscape, identify high-impact opportunities, and lead the responsible implementation of AI within your organization.
Foundational Methods: Neural Networks, Deep Learning and Reinforcement Learning
Understanding the core technologies that power Artificial Intelligence in Healthcare is the first step toward effective implementation. These methods provide the computational engine for analyzing complex medical data.
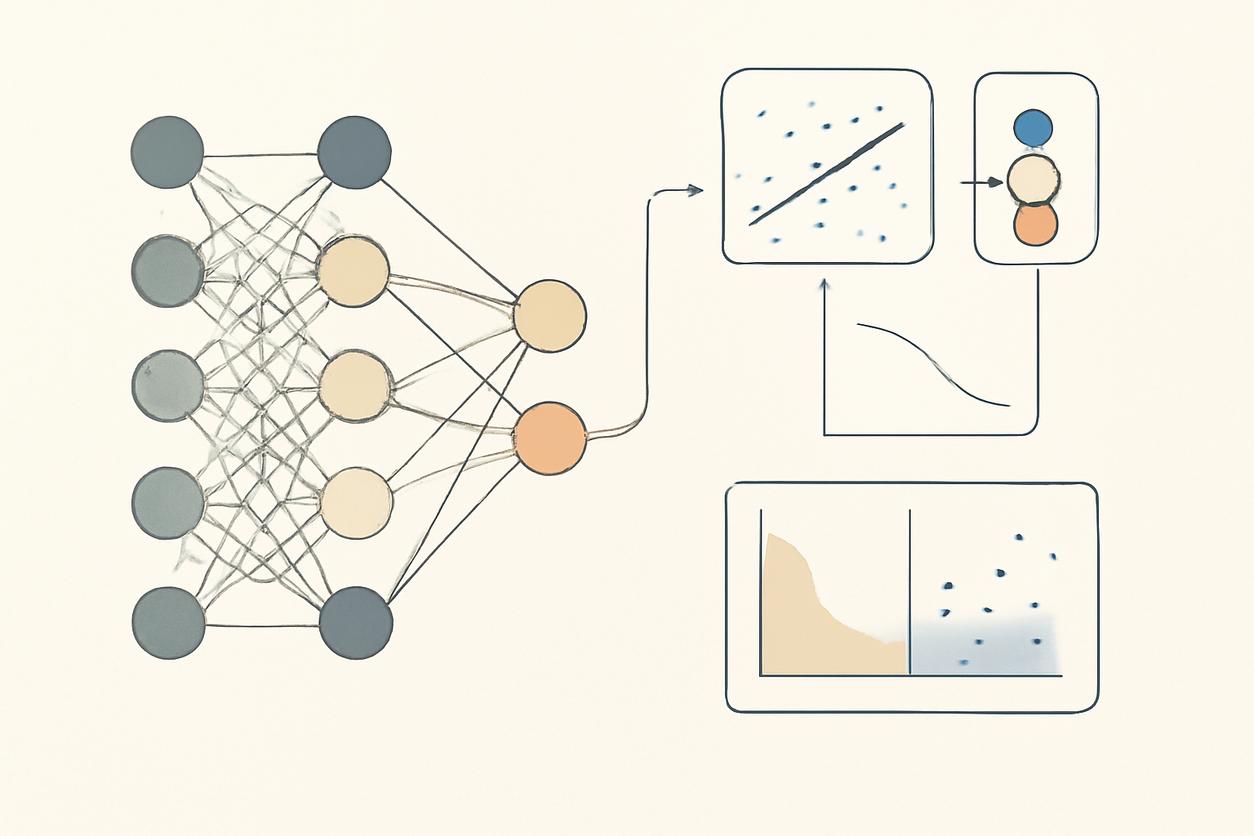
Neural Networks (NNs)
At their core, Neural Networks are computing systems inspired by the biological neural networks that constitute animal brains. They consist of interconnected nodes, or “neurons,” organized in layers. An input layer receives data, one or more hidden layers process it through a series of weighted connections, and an output layer delivers the final result, such as a classification or prediction. Their strength lies in learning non-linear relationships within data, making them versatile for a range of clinical tasks.
Deep Learning (DL)
Deep Learning is a subfield of machine learning based on neural networks with many layers—hence the term “deep.” This depth allows the model to learn hierarchical patterns from vast amounts of data. For instance, in an image, a deep learning model might first learn to identify simple edges, then combine them to recognize shapes, and ultimately identify complex objects like a tumor. This capability has made deep learning the dominant force in medical imaging analysis and other complex pattern recognition tasks within healthcare.
Reinforcement Learning (RL)
Unlike the pattern recognition focus of NNs and DL, Reinforcement Learning is concerned with decision-making. An RL agent learns to make a sequence of decisions in a dynamic environment to maximize a cumulative reward. In medicine, this could translate to optimizing a patient’s treatment protocol over time, where the “reward” is a positive health outcome. While still an emerging area, RL holds significant promise for developing dynamic treatment regimes and personalizing long-term care strategies.
Natural Language Processing for Clinical Text
A significant portion of valuable clinical information is locked within unstructured text, such as electronic health record (EHR) notes, pathology reports, and scientific literature. Natural Language Processing (NLP) is a branch of AI that gives computers the ability to understand, interpret, and generate human language, making this data accessible for analysis.
Key applications of NLP in the clinical domain include:
- Information Extraction: Automatically identifying and extracting key clinical concepts like diagnoses, medications, and lab values from free-text notes.
- Clinical Documentation Improvement (CDI): Analyzing clinical notes in real-time to suggest more precise diagnostic codes, improving billing accuracy and data quality.
- Cohort Identification for Research: Sifting through millions of patient records to find eligible candidates for clinical trials based on complex criteria described in their notes.
- Pharmacovigilance: Monitoring clinical notes and patient forums for mentions of adverse drug events that might not be formally reported.
Imaging and Signal Analysis: Beyond Radiology
While radiology was the first frontier for Artificial Intelligence in Healthcare imaging, its applications now span numerous specialties. AI algorithms, particularly those based on deep learning, can analyze medical images and physiological signals with a level of precision and speed that can augment human expertise.
Key application areas include:
- Radiology: Detection and classification of abnormalities in X-rays, CT scans, and MRIs, such as identifying cancerous nodules or flagging potential strokes.
- Pathology: Analyzing digital pathology slides to quantify biomarkers, grade tumors, and identify metastatic cells, reducing subjectivity and improving efficiency.
- Dermatology: Classifying skin lesions from photographs to assist in early melanoma detection.
- Cardiology: Interpreting electrocardiogram (ECG) and echocardiogram signals to predict cardiac events or detect arrhythmias that might be missed by the human eye.
Predictive Modeling for Patient Risk and Personalized Care
One of the most powerful applications of Artificial Intelligence in Healthcare is its ability to build predictive models that forecast future health events. By learning from historical data, these models can identify high-risk patients who may benefit from early intervention, paving the way for more proactive and personalized care.
Examples of predictive models in clinical use or advanced development include:
- Sepsis Prediction: Continuously monitoring patient vitals and lab results to provide early warnings for the onset of sepsis.
- Hospital Readmission Risk: Identifying patients at high risk of being readmitted within 30 days of discharge, allowing for targeted post-discharge support.
- Disease Progression Modeling: Predicting the likely course of chronic diseases like diabetes or chronic kidney disease for an individual patient.
- Treatment Response Prediction: Forecasting which patients are most likely to respond to a specific therapy, a cornerstone of personalized medicine.
Operational Automation: Clinical Workflow and Administrative Tasks
Beyond direct clinical care, AI offers substantial opportunities to improve the efficiency of healthcare operations. By automating repetitive and administrative tasks, AI can reduce costs, minimize errors, and, most importantly, free up clinicians’ time to focus on patient care.
Areas ripe for operational automation include:
- Patient Scheduling: Optimizing appointment schedules to minimize patient wait times and maximize resource utilization.
- Revenue Cycle Management: Automating medical coding, claims submission, and denial management to improve financial performance.
- Resource Allocation: Predicting patient flow and demand to optimize staffing levels and bed management in hospitals.
- Prior Authorization: Streamlining the cumbersome process of obtaining pre-approval from insurers for procedures and medications.
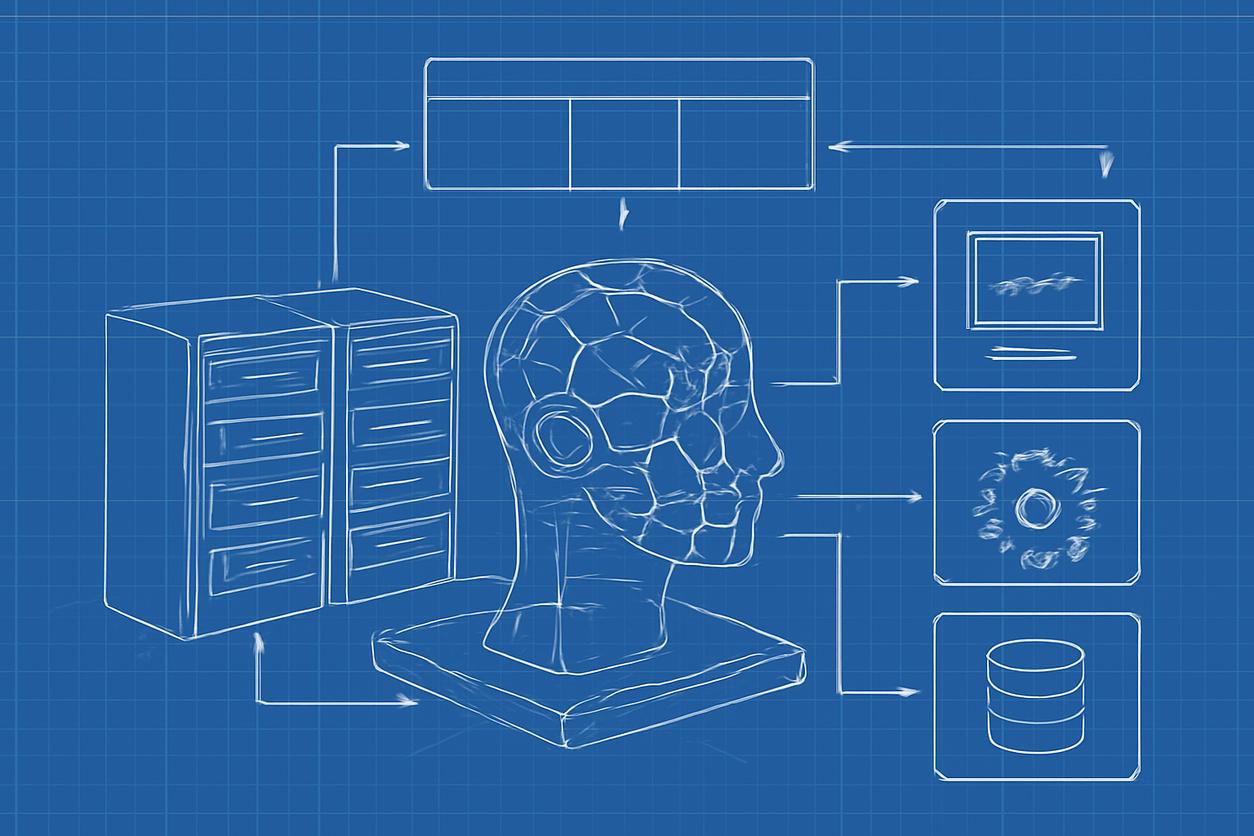
Data Quality, Standards and Interoperability
The performance of any AI model is fundamentally limited by the quality of the data it is trained on. For Artificial Intelligence in Healthcare, this principle of “garbage in, garbage out” is paramount. Achieving high-quality, interoperable data is the single most critical prerequisite for successful AI implementation.
Key considerations include:
- Data Quality: Data must be accurate, complete, consistent, and timely. This requires robust data governance programs and tools for data cleaning and validation.
- Data Standards: Adherence to common data models and terminologies (e.g., FHIR, OMOP, SNOMED CT, LOINC) is essential for ensuring that data from different sources can be combined and understood.
- Interoperability: Data often resides in siloed systems (EHRs, PACS, LIS). True interoperability—the seamless exchange of data between these systems—is necessary to create the comprehensive datasets required for powerful AI models.
Validation, Performance Metrics and Real-World Evaluation
A promising result in a lab setting does not guarantee clinical utility. Rigorous validation and a clear understanding of performance metrics are non-negotiable before deploying any AI tool in a live clinical environment.
Key Performance Metrics
It is crucial to select metrics that align with the clinical use case. Common metrics for classification models include:
| Metric | Definition | Clinical Relevance |
|---|---|---|
| Sensitivity (Recall) | The proportion of actual positives that are correctly identified (TP / (TP + FN)). | Crucial for screening tests where missing a disease has high consequences. |
| Specificity | The proportion of actual negatives that are correctly identified (TN / (TN + FP)). | Important to avoid over-treatment and unnecessary follow-up procedures. |
| Positive Predictive Value (PPV) | The proportion of positive predictions that are truly positive (TP / (TP + FP)). | Tells a clinician the probability that a positive AI finding is correct. |
| Area Under the ROC Curve (AUC-ROC) | A measure of the model’s ability to distinguish between classes across all thresholds. | Provides a single score to summarize overall model performance. |
Real-World Evaluation (RWE)
After internal validation, models must be tested in real-world clinical settings. This involves prospective studies to see how the model performs on new, unseen patient populations and how it integrates into the clinical workflow. Real-world evaluation helps answer the most important question: Does this AI tool actually improve patient outcomes, enhance efficiency, or reduce costs?
Ethical Safeguards and Responsible AI Governance
The power of Artificial Intelligence in Healthcare comes with profound ethical responsibilities. A robust governance framework is essential to ensure that AI is used safely, equitably, and transparently.
Core pillars of a responsible AI governance framework include:
- Fairness and Bias Mitigation: AI models can inherit and even amplify biases present in historical data. It is critical to audit models for performance disparities across different demographic groups (e.g., race, gender, socioeconomic status) and implement strategies to mitigate identified biases.
- Transparency and Explainability: Clinicians and patients need to understand why an AI model makes a particular recommendation. While some models are “black boxes,” techniques for explainable AI (XAI) are emerging to provide insight into the model’s decision-making process.
- Accountability: Clear lines of responsibility must be established. Who is accountable if an AI system contributes to a negative patient outcome—the developer, the hospital, or the clinician who used the tool?
- Human Oversight: For the foreseeable future, AI should be viewed as a tool to augment, not replace, human clinical judgment. A “human-in-the-loop” approach ensures that a qualified professional has the final say in patient care decisions.
Privacy, Security and Data Stewardship
Patient data is highly sensitive, and its use in AI systems requires an unwavering commitment to privacy and security. Healthcare organizations must act as responsible stewards of this data to maintain patient trust.
Key strategies include:
- Regulatory Compliance: All AI initiatives must strictly adhere to data protection regulations such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States.
- Data Security: Robust cybersecurity measures are needed to protect data from breaches, whether it is stored on-premise or in the cloud.
- Privacy-Preserving Techniques: Methods like de-identification (removing personal identifiers) and federated learning (training models locally without moving raw data) can train powerful AI models while minimizing privacy risks.
Implementation Roadmap: Pilot to Scale with Checklist
Moving from a concept to a fully integrated AI solution requires a structured, phased approach. A successful strategy for 2025 and beyond involves starting with a well-defined pilot project and scaling methodically.
Implementation Checklist for 2025+ Strategies
- 1. Problem and Use Case Definition: Clearly define a specific, high-impact clinical or operational problem that AI can solve. Avoid “AI for AI’s sake.”
- 2. Multidisciplinary Team Assembly: Form a core team that includes clinicians, data scientists, IT specialists, informaticists, and administrative leaders. Clinical buy-in from the start is essential.
- 3. Data Infrastructure and Readiness Assessment: Audit your data sources. Is the necessary data available, accessible, and of sufficient quality?
- 4. “Build vs. Buy” Decision: Evaluate whether to develop a model in-house or partner with a vendor. Consider your organization’s technical expertise, resources, and timeline.
- 5. Pilot Project Execution: Start with a small-scale pilot. Define clear success metrics before you begin. Focus on learning and iterating.
- 6. Rigorous Validation: Validate the model’s performance on your local patient population, not just the data it was trained on.
- 7. Clinical Workflow Integration Plan: Design exactly how the AI tool’s output will be presented to clinicians within their existing workflow (e.g., as an EHR alert). This is a critical and often overlooked step.
- 8. Post-Deployment Monitoring and Governance: Continuously monitor the model’s performance in the real world to watch for “model drift” and ensure it continues to perform safely and effectively.
Common Pitfalls and Mitigation Strategies
Many early initiatives in Artificial Intelligence in Healthcare falter due to predictable challenges. Awareness of these pitfalls is the first step toward avoiding them.
| Common Pitfall | Mitigation Strategy |
|---|---|
| Lack of a Clear Problem | Start with a clinical need, not a technology. Involve end-users (clinicians) from day one to define the problem. |
| Poor Data Quality or Access | Conduct a thorough data readiness assessment. Invest in data governance and infrastructure before launching major AI projects. |
| Failure to Secure Clinical Buy-in | Make clinicians partners in the development process. Ensure the AI tool solves a real problem for them and fits their workflow. |
| Ignoring Workflow Integration | Design the user interface and integration points with as much care as the algorithm itself. Use human-centered design principles. |
| Underestimating Validation Needs | Plan for rigorous, local, and prospective validation. Acknowledge that a model’s performance can vary between different populations. |
Emerging Trends: Autonomous Systems and Cognitive Computing
The field of Artificial Intelligence in Healthcare is continuously evolving. Looking ahead, two major trends are gaining momentum. Autonomous systems refer to AI that can perform tasks with minimal human oversight, such as automated insulin delivery systems. The ethical and safety considerations for such systems are immense. Cognitive computing aims to create systems that can simulate human thought processes to solve complex problems with ambiguity and uncertainty. This could lead to more sophisticated clinical decision support systems that act as true “cognitive assistants” for physicians. These advanced applications underscore the growing capabilities and future potential of AI in medicine.
Curated Resources and Further Reading
Staying current in this rapidly changing field is essential. The following resources provide access to high-quality research and information on Artificial Intelligence in Healthcare:
- PubMed: A free search engine accessing primarily the MEDLINE database of references and abstracts on life sciences and biomedical topics, maintained by the U.S. National Institutes of Health.
- National Institutes of Health (NIH): The primary agency of the United States government responsible for biomedical and public health research, often funding and publishing key studies on AI in medicine.
- World Health Organization (WHO): The WHO provides a global perspective on health, including guidance and reports on the ethical and policy implications of digital health technologies like AI.
- Journal of Medical Internet Research (JMIR): A leading peer-reviewed journal for digital medicine, health, and healthcare in the internet age, featuring many articles on AI applications.
- ArXiv AI Papers: A repository of electronic preprints of scientific papers in fields including computer science and AI, offering access to the latest cutting-edge research before formal publication.
Summary and Practical Next Steps
Artificial Intelligence in Healthcare is a powerful set of tools with the potential to fundamentally improve diagnostics, treatment, and operational efficiency. However, its successful adoption is not merely a technical challenge; it is a sociotechnical one. It requires a foundation of high-quality data, a commitment to rigorous validation, and an unwavering focus on ethical principles. The most successful implementations will be those that are clinically led, solve well-defined problems, and seamlessly integrate into the workflow to support, not supplant, human expertise.
For leaders ready to move forward, the next steps are clear:
- Educate and Build Consensus: Foster a common understanding of AI’s realistic capabilities and limitations among stakeholders in your organization.
- Establish Governance: Create a multidisciplinary AI governance committee to oversee ethical guidelines, data stewardship, and project prioritization.
- Identify a Pilot Project: Use the implementation checklist to select a high-impact, achievable first project that can demonstrate value and build momentum for future initiatives.
By taking a strategic, measured, and human-centered approach, healthcare organizations can harness the transformative power of AI to build a more efficient, effective, and equitable future for medicine.