Table of Contents
- Executive Summary
- Why Artificial Intelligence Matters in Modern Healthcare
- Core Concepts and Terminology
- High-Impact Clinical Applications
- Technical Building Blocks
- Data Stewardship and Governance
- Ethics and Responsible AI in Care
- Deployment Playbook and Checklist
- Measuring Impact and Outcomes
- Common Pitfalls and How to Avoid Them
- Roadmap and Emerging Directions
- Resources and Further Reading
Executive Summary
Artificial Intelligence in Healthcare is no longer a futuristic concept; it is a transformative force actively reshaping patient care, clinical operations, and medical research. This comprehensive guide serves as a practical playbook for healthcare leaders, clinicians, and data practitioners aiming to harness the power of AI. We will demystify core concepts, explore high-impact clinical applications, and detail the technical and governance frameworks necessary for successful implementation. From improving diagnostic accuracy in medical imaging to predicting patient deterioration, AI offers unprecedented opportunities to enhance efficiency, reduce costs, and, most importantly, improve patient outcomes. This article provides an actionable framework, including a deployment checklist, to help organizations navigate the complexities of integrating AI into clinical practice responsibly and effectively.
Why Artificial Intelligence Matters in Modern Healthcare
The healthcare industry is facing immense pressure from rising costs, aging populations, and an ever-increasing volume of complex patient data. Traditional models of care are struggling to keep pace. Artificial Intelligence in Healthcare offers a powerful solution by augmenting human expertise, automating repetitive tasks, and uncovering insights hidden within vast datasets. It empowers clinicians to make more informed decisions faster, enables personalized treatment plans, and streamlines administrative workflows. By shifting from reactive to proactive care, AI is a critical enabler of the move towards value-based healthcare, where the focus is on delivering better outcomes at a lower cost.
Clinical Problems Suited to Algorithmic Solutions
Not all clinical challenges are a good fit for AI. Algorithmic solutions excel at specific types of problems that are common in medicine. Understanding these categories helps in identifying the most promising opportunities for initial AI projects.
- Pattern Recognition: AI, particularly deep learning, is exceptionally skilled at identifying complex patterns in data that may be invisible to the human eye. This is highly applicable in radiology for spotting tumors in scans or in pathology for analyzing tissue samples.
- Prediction and Forecasting: Using historical data, AI models can predict future events. This includes forecasting patient readmission risks, identifying individuals likely to develop sepsis, or predicting disease progression.
- Optimization and Resource Allocation: AI can solve complex logistical challenges, such as optimizing operating room scheduling, managing hospital bed capacity, or personalizing patient treatment pathways for maximum efficacy.
- Data Synthesis and Extraction: AI can process and structure vast amounts of unstructured data, like clinical notes or medical literature, to extract meaningful information, reducing administrative burden and supporting evidence-based practice.
Core Concepts and Terminology
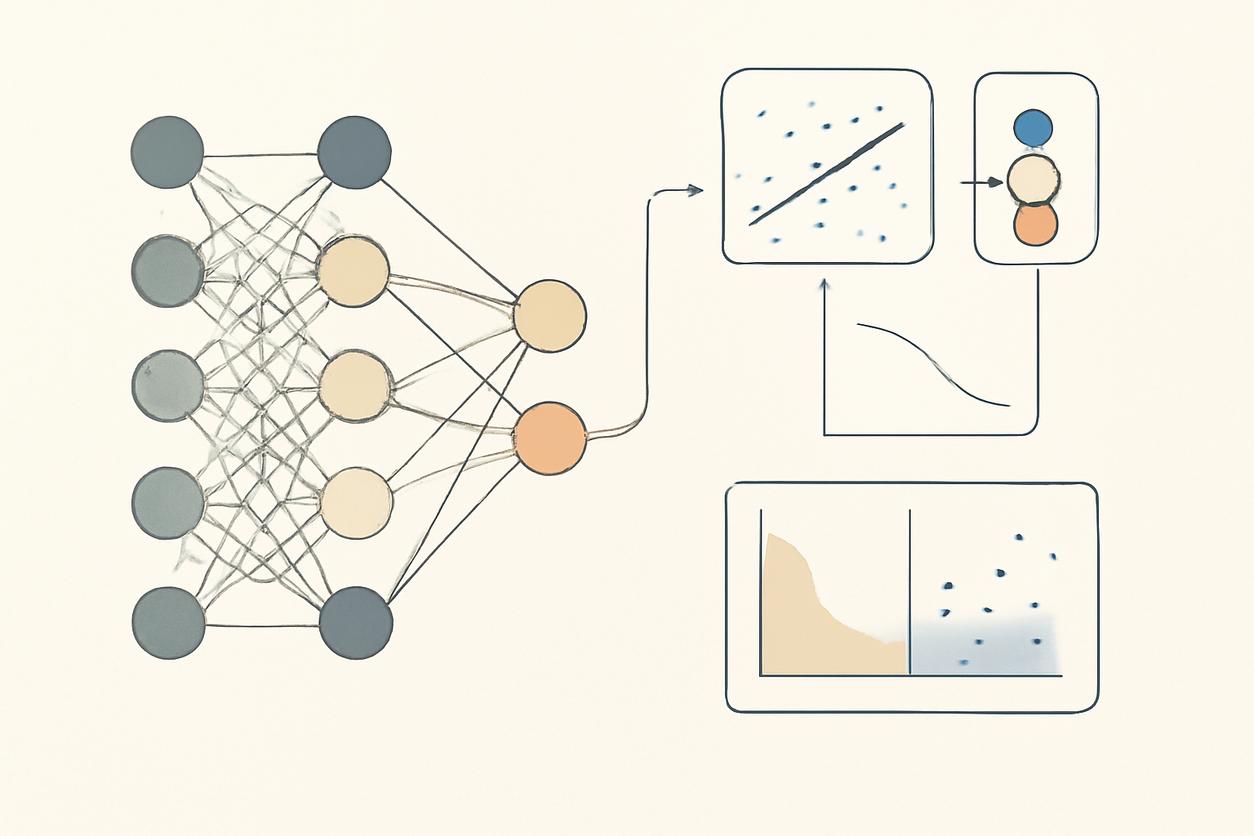
To effectively lead AI initiatives, a foundational understanding of key terminology is essential. Machine Learning (ML) is a subset of AI where systems learn from data to identify patterns and make decisions with minimal human intervention. Deep Learning is a further subset of ML that uses multi-layered neural networks to solve highly complex problems.
Neural networks, predictive modelling and natural language processing explained
These three concepts are the workhorses of modern artificial intelligence in healthcare.
- Neural Networks: Inspired by the human brain, these are computing systems made up of interconnected nodes, or neurons, organized in layers. They are the engine behind most deep learning breakthroughs and are particularly effective for tasks like image analysis and recognizing complex, non-linear patterns in patient data.
- Predictive Modeling: This is a statistical process of using known data to build a model that can reliably predict future outcomes. For example, a predictive model might use a patient’s electronic health record (EHR) data—including labs, vitals, and demographics—to calculate their risk of a heart attack within the next year.
- Natural Language Processing (NLP): NLP is a field of AI that gives computers the ability to read, understand, and derive meaning from human language. In healthcare, it is used to extract structured information from unstructured clinical notes, power chatbots for patient engagement, and summarize medical literature.
High-Impact Clinical Applications
The theoretical potential of artificial intelligence in healthcare is now being realized in tangible, high-impact applications across various clinical domains. These tools are designed not to replace clinicians, but to augment their capabilities and offload cognitive burdens.
Diagnostics and Imaging Workflows
AI algorithms are revolutionizing medical imaging analysis. In radiology and pathology, deep learning models can analyze X-rays, CT scans, and digital pathology slides to detect abnormalities like cancerous lesions or signs of diabetic retinopathy with a level of accuracy that can meet or exceed human performance. These tools act as a “second pair of eyes,” helping to prioritize urgent cases, reduce diagnostic errors, and accelerate turnaround times for reports.
Risk Stratification and Predictive Monitoring
One of the most powerful uses of AI is in predicting adverse events before they happen. Hospitals are deploying models that continuously monitor patient data from the EHR to identify those at high risk for conditions like sepsis, acute kidney injury, or in-hospital falls. These early warning systems allow clinical teams to intervene proactively, leading to better patient outcomes and reduced lengths of stay. Similar models are used in population health to identify patients who would benefit most from care management programs.
Clinical Documentation and Decision Support
Clinician burnout is a critical issue, driven in large part by administrative tasks and documentation. AI-powered tools are helping to alleviate this burden. Ambient clinical intelligence systems can listen to patient-doctor conversations and automatically generate clinical notes. Integrated decision support tools can provide real-time, evidence-based recommendations to clinicians at the point of care, helping to standardize practice and avoid potential medical errors.
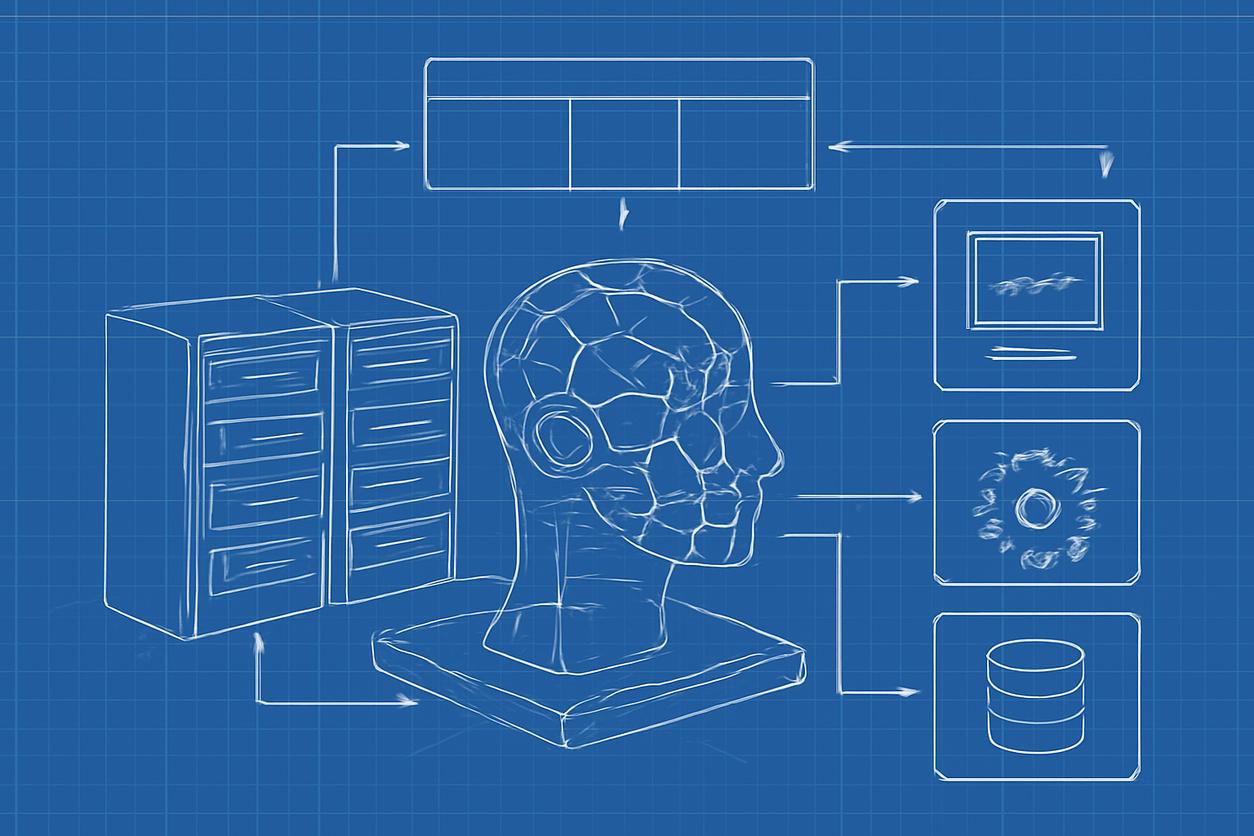
Technical Building Blocks
Deploying AI in a clinical setting requires a robust technical foundation. It is not just about the algorithm; it is about the entire data ecosystem that supports its development, validation, and operation.
Data Pipelines and Feature Engineering
High-quality, well-curated data is the lifeblood of any AI model. A data pipeline is the automated process of extracting, transforming, and loading (ETL) data from source systems like the EHR into a format suitable for model training. Feature engineering is the critical step of selecting and transforming the raw data variables (features) that the model will use to make predictions. This requires deep domain expertise to ensure the features are clinically relevant and meaningful.
Model Selection and Validation Strategies
There is no one-size-fits-all AI model. The choice of algorithm—from a simple logistic regression to a complex neural network—depends on the specific problem, the nature of the data, and the need for interpretability. Rigorous validation is non-negotiable. This involves testing the model on a dataset it has never seen before (a hold-out or validation set) to ensure it generalizes well and is not simply “memorizing” the training data. Prospective validation, where the model’s performance is tested on live data in a silent mode before clinical deployment, is a best practice.
Data Stewardship and Governance
The use of sensitive patient data for AI development mandates an uncompromising commitment to governance, privacy, and security. A strong governance framework is essential for building trust with patients, clinicians, and regulators.
Privacy, Deidentification, and Secure Data Handling
All AI projects must comply with regulations like HIPAA in the United States or GDPR in Europe. This requires robust protocols for deidentification, the process of removing personally identifiable information (PII) from datasets used for training. Data must be handled in secure, access-controlled environments, and techniques like differential privacy or federated learning can provide additional layers of protection by allowing models to be trained without centralizing sensitive data.
Interoperability and Standards
AI models are only useful if they can access data and integrate into clinical workflows. This requires adherence to interoperability standards. Key standards include:
- HL7 (Health Level Seven): A set of international standards for the transfer of clinical and administrative data between software applications.
- FHIR (Fast Healthcare Interoperability Resources): A next-generation standard from HL7 that uses modern web technologies to make data exchange simpler and faster.
- DICOM (Digital Imaging and Communications in Medicine): The universal standard for handling, storing, and transmitting medical images.
Ethics and Responsible AI in Care
Beyond technical accuracy, the ethical implications of using artificial intelligence in healthcare are paramount. An AI system that is technically sound but biased or opaque can cause real harm. A commitment to Responsible AI is a prerequisite for any healthcare organization.
Bias Auditing and Transparent Explanation
AI models learn from historical data, and if that data reflects existing societal or clinical biases, the model will perpetuate and even amplify them. Bias auditing is the process of systematically testing a model to ensure it performs fairly and equitably across different demographic groups (e.g., race, gender, socioeconomic status). Furthermore, many complex models operate as “black boxes.” The field of Explainable AI (XAI) is focused on developing techniques to make model predictions understandable to clinicians, fostering trust and enabling them to appropriately override the AI’s suggestion when clinically indicated. For a broader view on principles, see the AI Ethics and Governance guidelines.
Deployment Playbook and Checklist
Moving an AI model from a research environment to live clinical use is a complex undertaking. This playbook provides a structured approach to navigate the process successfully.
Pilot Design, Integration, and Clinician Training
Before a full-scale rollout, a well-designed pilot is crucial. Define a clear clinical problem, select a motivated clinical champion, and establish specific success metrics from the outset. Integration into the existing workflow (e.g., as a notification in the EHR) is key to adoption; the tool must make the clinician’s job easier, not harder. Training should focus not just on the technical aspects of the tool but on building clinical context: when to trust the model, when to be skeptical, and how its output fits into the overall clinical picture.
Operationalizing Monitoring and Model Updates
Deployment is not the end of the journey. Once live, models must be continuously monitored for performance degradation or “model drift,” which can occur as patient populations or clinical practices change. For strategies beginning in 2025 and beyond, organizations must have a clear plan for retraining and updating models periodically. This process, known as MLOps (Machine Learning Operations), ensures the AI tool remains safe, effective, and reliable over time.
Implementation Checklist
- Phase 1: Foundation and Scoping
- [ ] Identify a clear clinical or operational problem.
- [ ] Secure executive sponsorship and a clinical champion.
- [ ] Assemble a cross-functional team (clinical, IT, data science, legal).
- [ ] Conduct a data availability and quality assessment.
- [ ] Define clear success metrics (clinical, operational, financial).
- Phase 2: Development and Validation
- [ ] Develop secure data pipeline and feature engineering process.
- [ ] Train and internally validate the model.
- [ ] Perform a thorough bias and fairness audit.
- [ ] Conduct a prospective “silent mode” validation.
- Phase 3: Pilot and Deployment
- [ ] Design the clinical workflow integration.
- [ ] Develop a comprehensive training plan for end-users.
- [ ] Launch a limited-scope clinical pilot.
- [ ] Collect feedback and iterate on the workflow.
- Phase 4: Monitoring and Governance
- [ ] Implement a real-time performance monitoring dashboard.
- [ ] Establish a formal governance committee for the AI tool.
- [ ] Schedule regular model performance reviews and plan for retraining (e.g., annual reviews starting in 2026).
Measuring Impact and Outcomes
To justify investment and prove value, the impact of any AI initiative must be rigorously measured. A balanced scorecard approach, looking at multiple domains, is most effective.
Clinical, Operational and Economic Metrics
- Clinical Metrics: These measure the direct impact on patient care. Examples include reduced mortality rates for sepsis, lower hospital-acquired infection rates, or improved diagnostic accuracy.
- Operational Metrics: These measure the impact on efficiency and workflow. Examples include reduced average length of stay, faster report turnaround times in radiology, or decreased clinician documentation time.
- Economic Metrics: These measure the financial impact. Examples include cost savings from prevented adverse events, reduced readmission penalties, or improved resource utilization.
Common Pitfalls and How to Avoid Them
Many AI in healthcare projects fail to move beyond the pilot stage. Avoiding common pitfalls can significantly increase the chances of success.
- Solving the Wrong Problem: Focusing on a technically interesting problem instead of a pressing clinical need. Solution: Involve clinicians from day one to ensure the project is grounded in a real-world challenge.
- Poor Data Quality: “Garbage in, garbage out.” Using incomplete or inaccurate data will lead to a poor model. Solution: Invest heavily in data cleaning, validation, and governance before model development begins.
- Ignoring the Workflow: Building a highly accurate model that is too cumbersome for clinicians to use. Solution: Design the user interface and workflow integration with constant feedback from end-users.
- Lack of Trust: Deploying a “black box” model that clinicians do not understand or trust. Solution: Prioritize explainability and provide thorough training on the model’s strengths and limitations.
Roadmap and Emerging Directions
The field of artificial intelligence in healthcare is evolving rapidly. Looking ahead, several trends are poised to have a significant impact. Federated learning will allow models to be trained across multiple institutions without sharing sensitive patient data, leading to more robust and generalizable models. Generative AI, including large language models, holds immense promise for further revolutionizing clinical documentation, medical education, and patient communication. Finally, the concept of Reinforcement Learning may one day be used to optimize complex, long-term treatment policies for chronic diseases.
Resources and Further Reading (annotated)
- WHO Guidance on AI for Health: The Responsible AI page from the World Health Organization provides a global perspective on the ethical considerations and governance principles for AI in healthcare.
- OECD AI Principles: The AI Ethics and Governance framework from the OECD offers a set of intergovernmental policy guidelines for trustworthy AI that are highly relevant to healthcare applications.
- Wikipedia Overviews: For a deeper technical dive into core concepts, the articles on Neural Networks, Predictive Modeling, and Natural Language Processing provide excellent, well-referenced starting points.