The Clinician’s Guide to Artificial Intelligence in Healthcare: A Practical Whitepaper for Implementation and Innovation
Table of Contents
- Introduction: Why Machine Intelligence Matters in Care Delivery
- Real-World Clinical Applications and Tangible Outcomes
- Interpreting Model Outputs and Achieving Explainability
- Safeguarding Patient Data and Security Best Practices
- Regulatory Considerations and Compliance Pathways
- Validation, Monitoring, and Clinical Performance Metrics
- Practical Deployment Roadmap for Health Providers
- Short Clinician Case Studies and Lessons Learned
- Research Gaps and Near-Term Innovation Opportunities
- Appendix: Checklist for Pilot Projects and Evaluation Templates
- Further Reading and Curated Resources
Introduction: Why Machine Intelligence Matters in Care Delivery
As a practicing clinician, the term Artificial Intelligence in Healthcare can evoke a mix of excitement and skepticism. We are trained to rely on evidence, experience, and the nuanced art of medicine. The idea of an algorithm influencing patient care can feel abstract, even concerning. Yet, the reality is that the immense complexity and volume of modern medical data have surpassed the limits of human cognitive capacity. The true promise of AI is not to replace the clinician but to augment our abilities—to serve as a tireless, data-driven partner that can help us detect disease earlier, personalize treatment more effectively, and alleviate the administrative burdens that contribute to burnout. This whitepaper serves as a practical guide for clinicians, administrators, and data scientists, bridging the gap between the technical underpinnings of AI and its real-world application at the point of care.
Real-World Clinical Applications and Tangible Outcomes
The application of Artificial Intelligence in Healthcare is moving rapidly from theoretical research to tangible clinical tools that improve patient outcomes and operational efficiency. These are not future concepts; they are being deployed and refined in leading health systems today.
Diagnostic Imaging and Pattern Recognition Explained
One of the most mature applications of AI is in medical imaging. At its core, this technology uses a type of AI called a Convolutional Neural Network (CNN), which is designed to recognize patterns in visual data. For a radiologist, this is analogous to how a medical student learns to identify pathologies on an X-ray, but on a massive scale.
- Radiology: AI models can screen chest X-rays for signs of pneumonia or flag subtle nodules on a CT scan that may indicate early-stage lung cancer. These tools act as a second reader, enhancing diagnostic accuracy and reducing miss rates.
- Pathology: In digital pathology, AI can analyze high-resolution slide images to quantify tumor-infiltrating lymphocytes or identify regions with a high probability of malignancy, helping to grade cancers more consistently.
- Dermatology: Mobile applications are now capable of analyzing smartphone images of skin lesions to assess the risk of melanoma, providing a powerful triage tool for early detection.
Personalized Care Pathways Driven by Predictive Models
Beyond imaging, predictive analytics are transforming how we approach treatment planning. These models ingest vast, heterogeneous datasets—including EHR data, genomic information, and lab results—to forecast individual patient trajectories. The goal is to move from a one-size-fits-all approach to precision medicine.
- Oncology: AI can analyze a patient’s tumor genomics and clinical history to predict their likely response to different chemotherapy regimens or immunotherapies, guiding oncologists toward the most effective, least toxic treatment plan.
- Chronic Disease Management: For patients with diabetes, predictive models can analyze glucose monitoring data, diet, and activity levels to forecast hypoglycemic events, allowing for proactive adjustments to insulin dosing.
Population Health and Risk Stratification Use Cases
Scaling these predictive capabilities allows healthcare organizations to manage the health of entire populations. By identifying at-risk individuals before they become acutely ill, providers can implement targeted, preventative interventions. This is a cornerstone of value-based care.
- Sepsis Prediction: In the inpatient setting, AI systems continuously monitor vital signs and lab results from the EHR to calculate a patient’s real-time risk of developing sepsis. An alert integrated into the clinical workflow can trigger early intervention protocols, which has been shown to significantly reduce mortality.
- Readmission Risk: Upon discharge, models can predict a patient’s likelihood of being readmitted within 30 days. High-risk patients can be enrolled in enhanced transitional care programs, receiving follow-up calls, home health visits, or remote monitoring to ensure a safe recovery.
Operational Automation in Clinical Workflows
The burden of administrative tasks is a major driver of clinician burnout. Artificial Intelligence in Healthcare offers powerful solutions to automate and streamline these workflows, freeing up clinicians to focus on patient care.
- Ambient Clinical Intelligence: Systems that use natural language processing to listen to a patient-doctor conversation and automatically generate a structured clinical note in the EHR.
- Smart Scheduling: Optimizing outpatient appointment schedules to minimize patient wait times and maximize resource utilization based on predicted appointment lengths and patient needs.
- Bed Management: Predicting patient discharge times and inpatient admission surges to help hospitals manage bed capacity more efficiently.
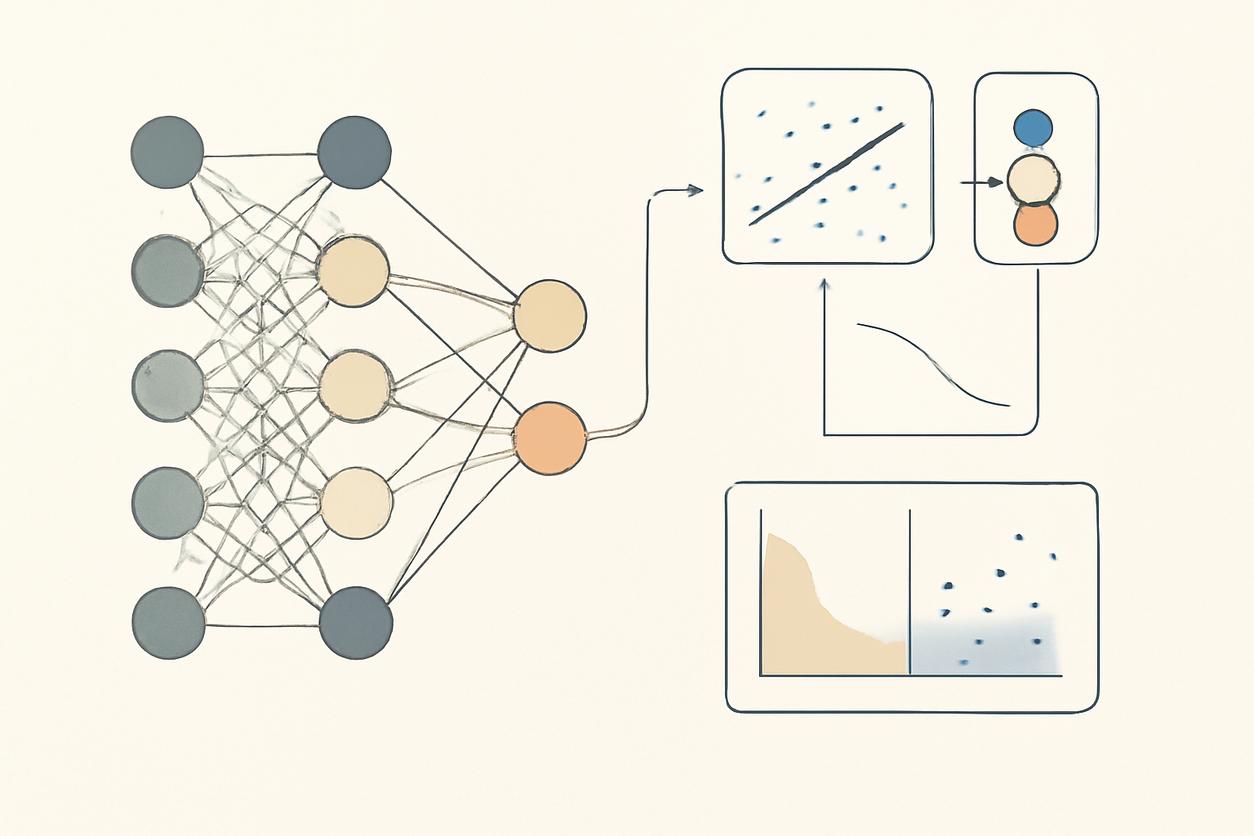
Interpreting Model Outputs and Achieving Explainability
For any AI tool to be trusted and adopted by clinicians, its recommendations cannot come from an inscrutable “black box.” The field of explainable AI (XAI) is dedicated to making model decision-making transparent. Instead of just providing an answer (e.g., “high risk of sepsis”), an explainable model shows its work. For instance, it might highlight the specific variables that contributed most to its risk score, such as a rising lactate level, a sudden drop in blood pressure, and an elevated white blood cell count. This transparency allows clinicians to use their judgment to validate or override the AI’s suggestion, maintaining clinical autonomy and ensuring patient safety.
Safeguarding Patient Data and Security Best Practices
Patient trust is paramount. The use of AI is contingent on robust data security and privacy. All projects must adhere to strict regulatory frameworks like HIPAA in the United States or GDPR in Europe. Key strategies include:
- Data De-identification: Removing all 18 HIPAA-defined personal identifiers before data is used for model training.
- Access Control: Implementing strict, role-based access to ensure that only authorized personnel can view or use sensitive patient data.
- Federated Learning: A cutting-edge technique where an AI model can be trained across multiple hospitals without the patient data ever leaving its source institution. The model “travels” to the data, not the other way around, preserving privacy while enabling the creation of more robust and diverse models.
Regulatory Considerations and Compliance Pathways
Many AI tools used for diagnosis or treatment are classified by regulatory bodies like the U.S. Food and Drug Administration (FDA) as Software as a Medical Device (SaMD). These products require rigorous validation and pre-market approval. The regulatory landscape for Artificial Intelligence in Healthcare is constantly evolving. Health systems must stay informed about guidelines for aspects like pre-determined change control plans, which allow models to be updated with new data, and real-world performance monitoring. Engaging with regulatory experts early in the development process is critical for a successful and compliant deployment. For global perspectives, resources from the World Health Organization provide guidance on the ethics and governance of AI for health.
Validation, Monitoring, and Clinical Performance Metrics
A model that performs well in a lab setting may not perform as expected in a real-world clinical environment. Rigorous validation is essential before, during, and after deployment.
- Initial Validation: The model must be tested on a local, retrospective dataset that is separate from its training data to ensure it generalizes well to the institution’s specific patient population.
- Performance Metrics: Key metrics include sensitivity (ability to correctly identify patients with the condition), specificity (ability to correctly identify patients without the condition), Positive Predictive Value (PPV), and the Area Under the Receiver Operating Characteristic (AUC-ROC) curve.
- Continuous Monitoring: Once deployed, the model’s performance must be continuously monitored for “model drift”—a degradation in performance that can occur as patient populations, care protocols, or data-gathering practices change over time. This includes actively monitoring for biases to ensure the model performs equitably across all demographic groups.
Practical Deployment Roadmap for Health Providers
Successfully integrating AI requires a strategic, multi-disciplinary approach. A practical roadmap for a health provider planning implementation in 2026 and beyond should prioritize clinical value and safety.
- Identify a High-Impact Clinical Problem: Start with a clear, well-defined problem where AI can provide a solution (e.g., reducing diagnostic errors for a specific condition, predicting patient deterioration).
- Assemble a Cross-Functional Team: The team must include clinicians who will use the tool, informaticians, data scientists, IT staff, and administrative leadership.
- Ensure Data Governance and Infrastructure: Confirm that high-quality, relevant data is accessible and that the necessary computational infrastructure is in place.
- Select or Develop the Right Tool: Decide whether to partner with a vendor or develop a solution in-house, ensuring the tool meets explainability and integration requirements.
- Conduct a Rigorous Pilot Project: Deploy the tool in a limited, controlled environment. Focus on workflow integration, clinical utility, and safety.
- Measure, Validate, and Iterate: Use the metrics defined in the previous section to evaluate the pilot. Gather feedback from end-users to refine the tool and workflow before considering a broader rollout.
Short Clinician Case Studies and Lessons Learned
From my own observations and conversations with colleagues, the successes and failures of AI implementation often hinge on human factors.
- A Radiologist’s Perspective: “We trialed an AI tool for flagging intracranial hemorrhages on head CTs. Initially, the high number of false positives created significant ‘alert fatigue.’ We worked with the developers to adjust the model’s sensitivity threshold. The key lesson was that the tool’s clinical utility depended entirely on how well it was calibrated to our specific workflow and tolerance for false alerts. It’s not just about accuracy; it’s about usability.”
- An ICU Nurse’s Perspective: “The sepsis prediction alert was a game-changer, but only after we integrated it directly into our rounding checklists. At first, it was just another alarm going off. By making it a mandatory discussion point during rounds for high-risk patients, we turned a passive alert into an active clinical decision-support tool. The lesson is that implementation is as much a process-change challenge as it is a technology challenge.”
Research Gaps and Near-Term Innovation Opportunities
The field of Artificial Intelligence in Healthcare is advancing rapidly, yet significant challenges and opportunities remain. Future innovation will likely focus on:
- Multi-Modal Data Fusion: Developing models that can simultaneously analyze and learn from different data types—such as imaging, genomics, clinical notes, and real-time sensor data—to create a more holistic and accurate picture of a patient’s health.
- Causality and Counterfactuals: Moving beyond correlation to understand causation. Future models may be able to answer questions like, “What would this patient’s outcome have been if we had chosen treatment B instead of treatment A?”
- Generative AI for Synthetic Data: Using generative models to create realistic but artificial patient data. This could revolutionize research and model training by providing large, perfectly-labeled datasets without compromising the privacy of real patients. For the latest breakthroughs, journals like Nature Medicine AI are invaluable resources.
Appendix: Checklist for Pilot Projects and Evaluation Templates
Checklist for AI Pilot Projects
- Problem Definition: Is the clinical problem specific, measurable, and important to our patients and organization?
- Team Composition: Does our project team include clinical champions, IT, data science, and administrative support?
- Data Readiness: Do we have access to sufficient high-quality, relevant, and representative data for training and validation?
- Ethical and Bias Review: Have we conducted a formal review for potential biases and established a fairness monitoring plan?
- Workflow Integration: How will the AI tool’s output be presented to the clinician? Does it fit seamlessly into the existing workflow?
- Metrics for Success: Have we defined clear metrics for success, including clinical outcomes (e.g., mortality, length of stay), operational metrics (e.g., clinician time saved), and model performance metrics (e.g., accuracy, sensitivity)?
- Clinician Training: Is there a comprehensive plan to train end-users on how to use the tool and interpret its outputs correctly?
AI Tool Evaluation Template
| Evaluation Domain | Key Questions | Rating (1-5) |
|---|---|---|
| Clinical Validity | Does the tool accurately detect, predict, or classify the target clinical concept? Is there strong evidence from peer-reviewed studies? | |
| Clinical Utility | Does using the tool lead to improved patient outcomes or a more efficient care process? Does it provide actionable information? | |
| Usability and Workflow Integration | Is the tool easy to use? Does it integrate with our existing EHR and clinical workflows without causing disruption or alert fatigue? | |
| Explainability and Trust | Does the tool provide clear explanations for its outputs? Do clinicians understand why it is making a particular recommendation? | |
| Fairness and Equity | Has the tool been validated for performance across different demographic subgroups within our patient population? |
Further Reading and Curated Resources
Staying current in this dynamic field is essential. The following resources provide high-quality, evidence-based information on Artificial Intelligence in Healthcare.
- PubMed: The primary source for peer-reviewed clinical research and validation studies on AI applications. A targeted search can yield the latest evidence for specific clinical use cases.
- National Institutes of Health (NIH): Offers information on federally funded research initiatives, strategic plans, and data science resources related to AI in medicine.
- World Health Organization (WHO): Provides a global perspective on the ethical considerations, governance, and policy-making for AI in health and medicine.
- Nature Medicine AI: A collection of cutting-edge research, reviews, and commentary on the latest breakthroughs in medical AI from a leading scientific publisher.